How to Become a Physical Therapist: A Complete Guide
Table of Contents
Learning how to become a physical therapist is the first step toward a rewarding career dedicated to restoring function, reducing pain, and improving lives. As healthcare evolves, so do the physical therapist education requirements. This guide provides a comprehensive overview of the pathway to getting your PT licensure in the United States.
We will cover the academic steps, DPT program requirements, the NPTE exam, and how modern tools like HelloNote EMR support new graduates as they begin their careers.
Step 1: Laying the Foundation – The Bachelor’s Degree
The first major step is earning a bachelor’s degree from an accredited university. While there is no single required major, success hinges on completing prerequisite coursework. Common majors include Kinesiology, Biology, and Health Sciences.
Mastering DPT Program Prerequisites
Anatomy & Physiology (2 semesters with labs)
General Chemistry (2 semesters with labs)
General Physics (2 semesters with labs)
Biology (additional general or cellular courses)
Psychology (general, developmental, or abnormal)
Statistics
Admission is highly competitive. A strong GPA (often 3.5+) and direct observation hours in various clinical settings are critical to strengthening your application.
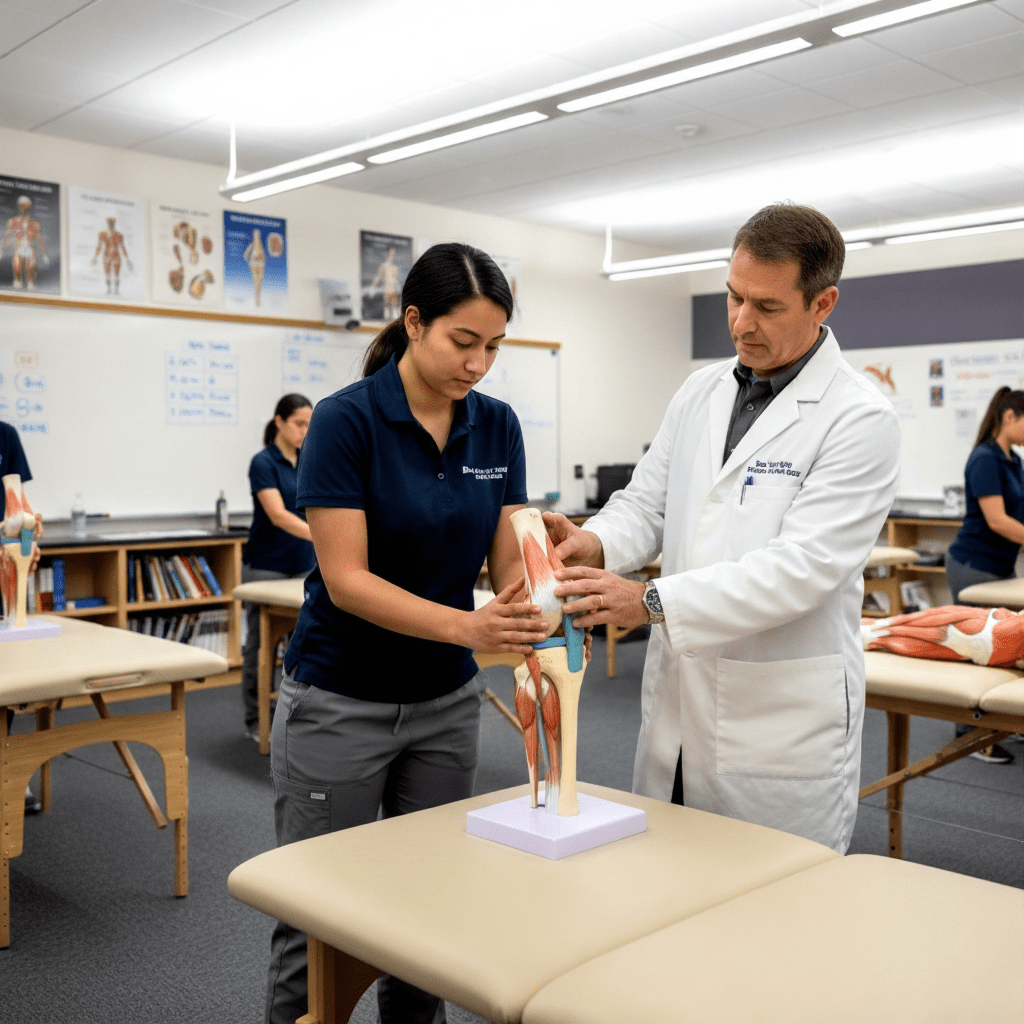
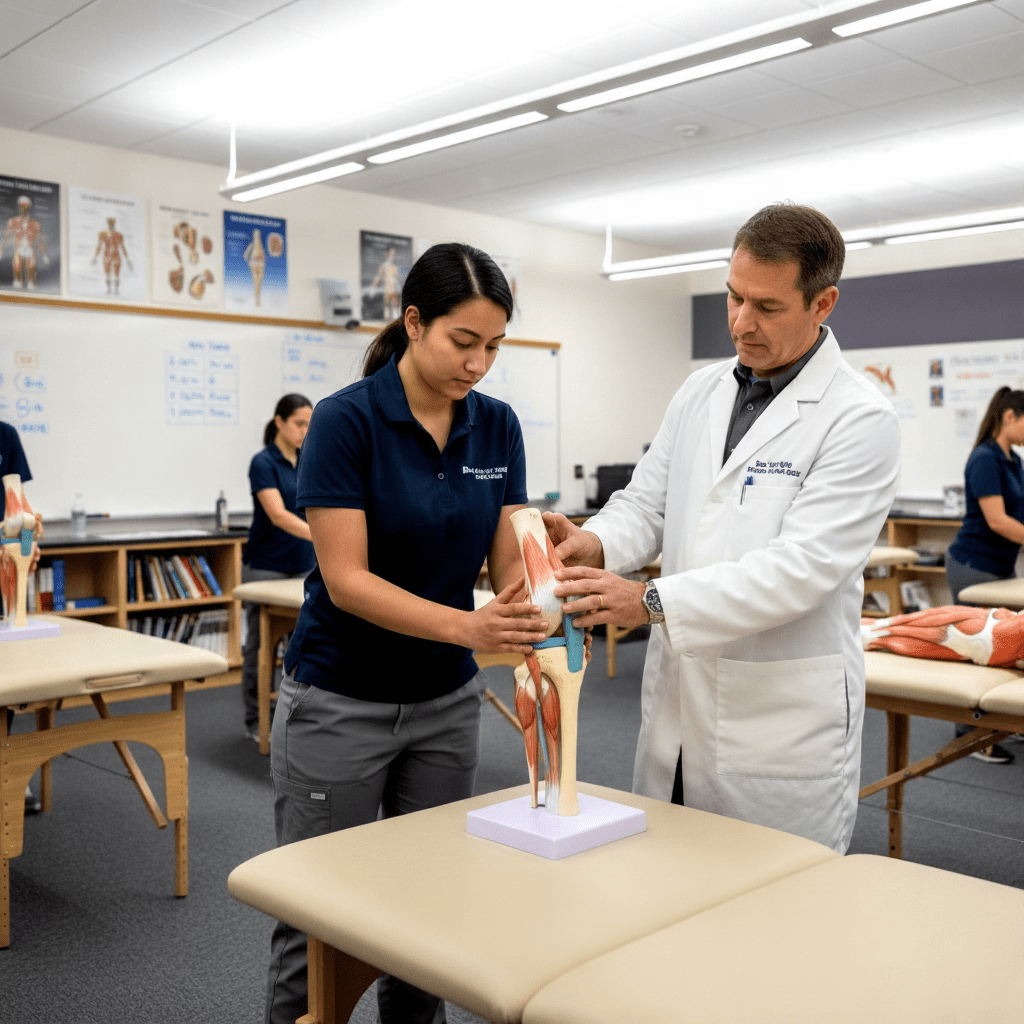
Step 2: Professional Training – The Doctor of Physical Therapy (DPT) Program
The cornerstone of physical therapy education is graduating from a Doctor of Physical Therapy (DPT) program, which typically takes three years.
The Critical Role of CAPTE Accreditation
It is imperative to attend a program accredited by the Commission on Accreditation in Physical Therapy Education (CAPTE). Graduation from a CAPTE-accredited program is required to sit for the national licensure exam.
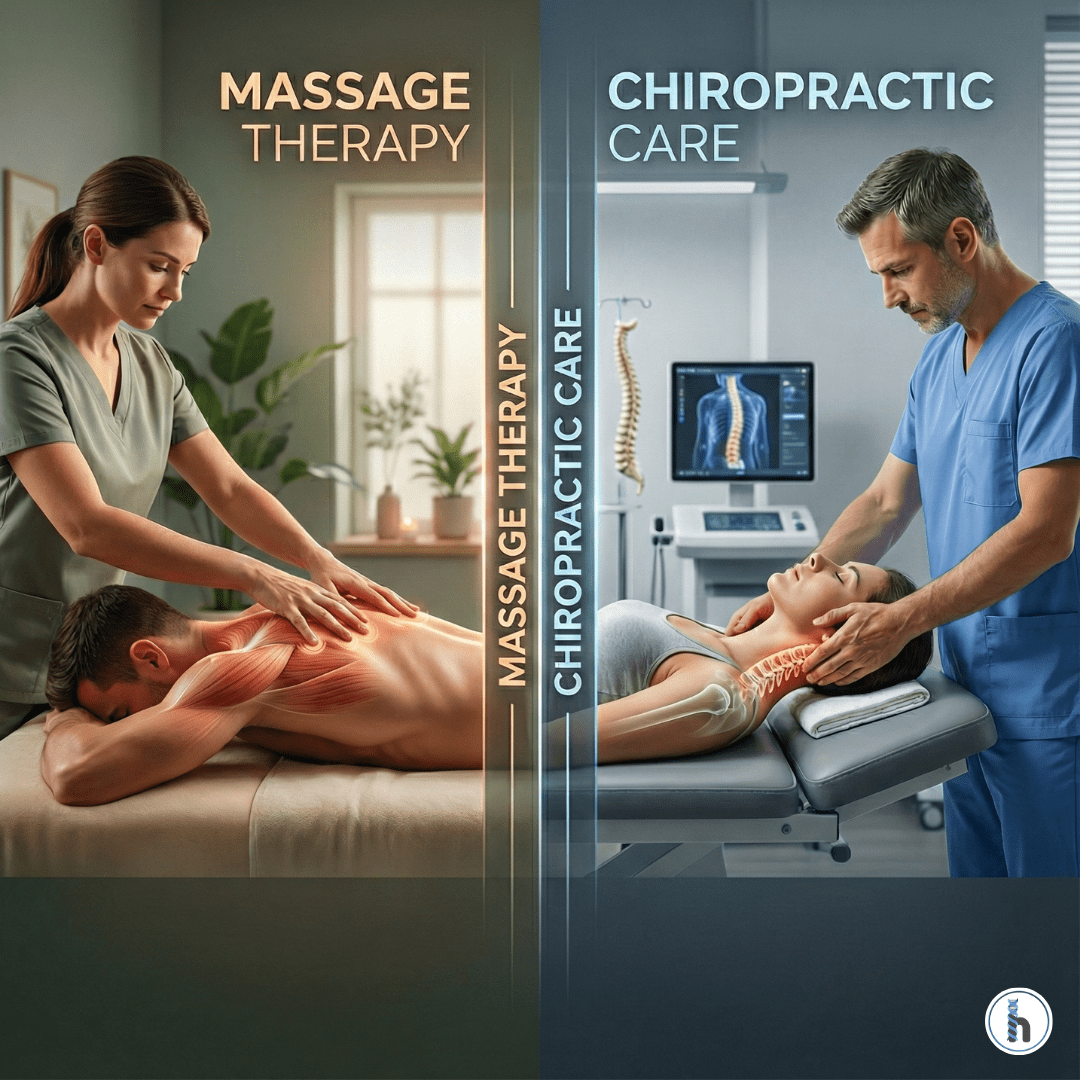
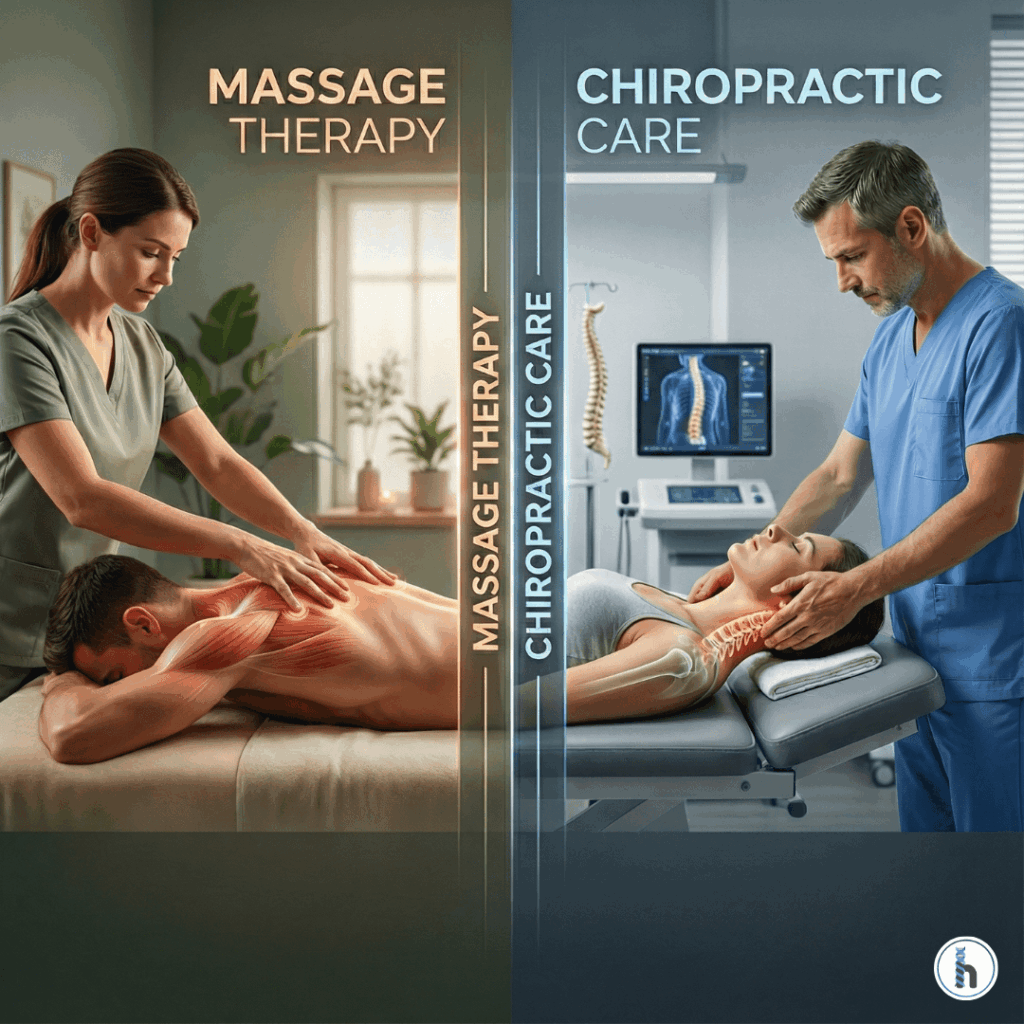
The DPT curriculum combines advanced coursework with over 30 weeks of full-time clinical rotations in diverse settings like orthopedic clinics, acute care hospitals, and pediatric centers.
Step 3: Demonstrating Competency – The NPTE Exam
After graduation, you must pass the National Physical Therapy Examination (NPTE), administered by the Federation of State Boards of Physical Therapy (FSBPT). This 250-question, 5-hour exam assesses the entry-level knowledge required to practice safely. A scaled score of 600 out of 800 is generally the minimum required to pass.
Step 4: Earning the Right to Practice – State PT Licensure
Passing the NPTE makes you eligible for your PT licensure, but each state has its own specific rules. These often include passing a jurisprudence exam on the state’s practice act and undergoing a criminal background check. Always consult the physical therapy licensing board for the specific state where you intend to work.
Step 5: Advancing Expertise – Optional Residency and Specialization
While not required, many licensed PTs pursue post-professional residency programs to accelerate their skills. This prepares them for board certification in one of the ten specialty areas recognized by the American Board of Physical Therapy Specialties (ABPTS).
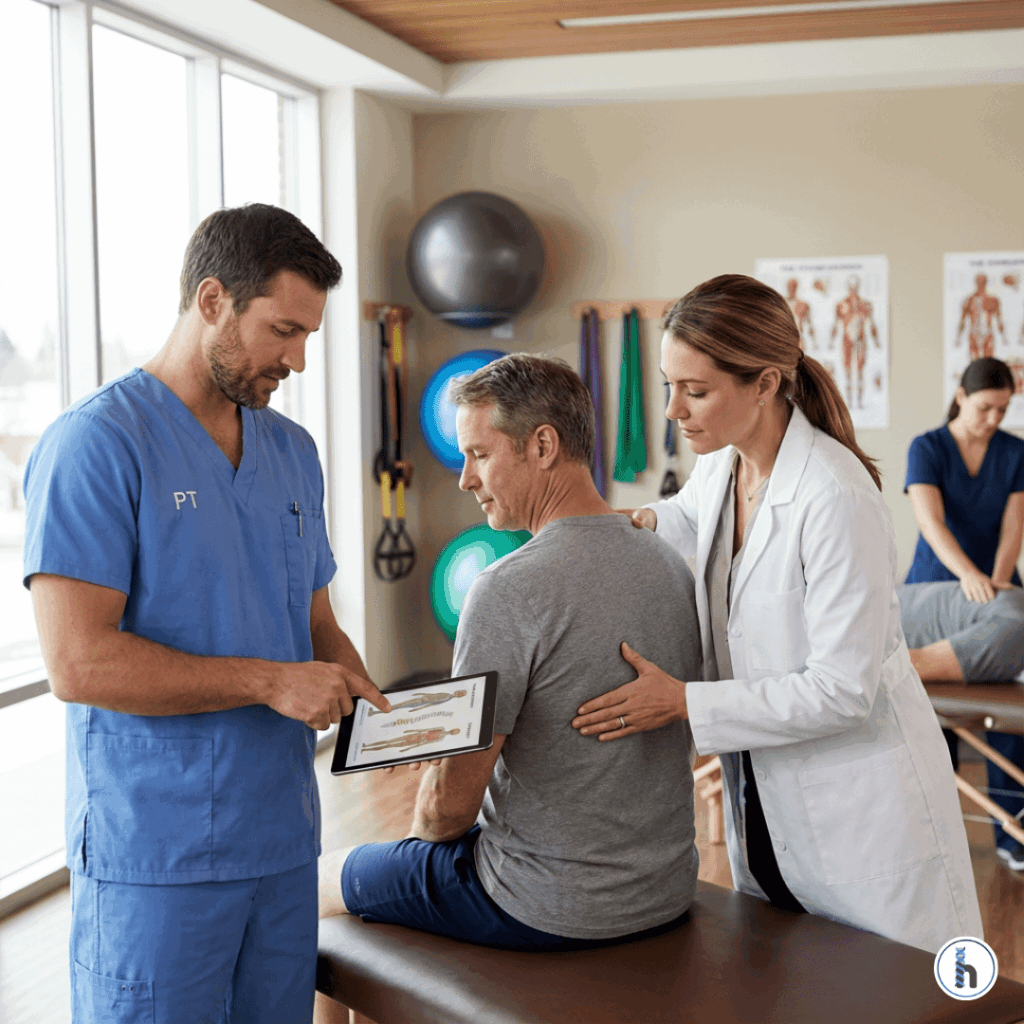
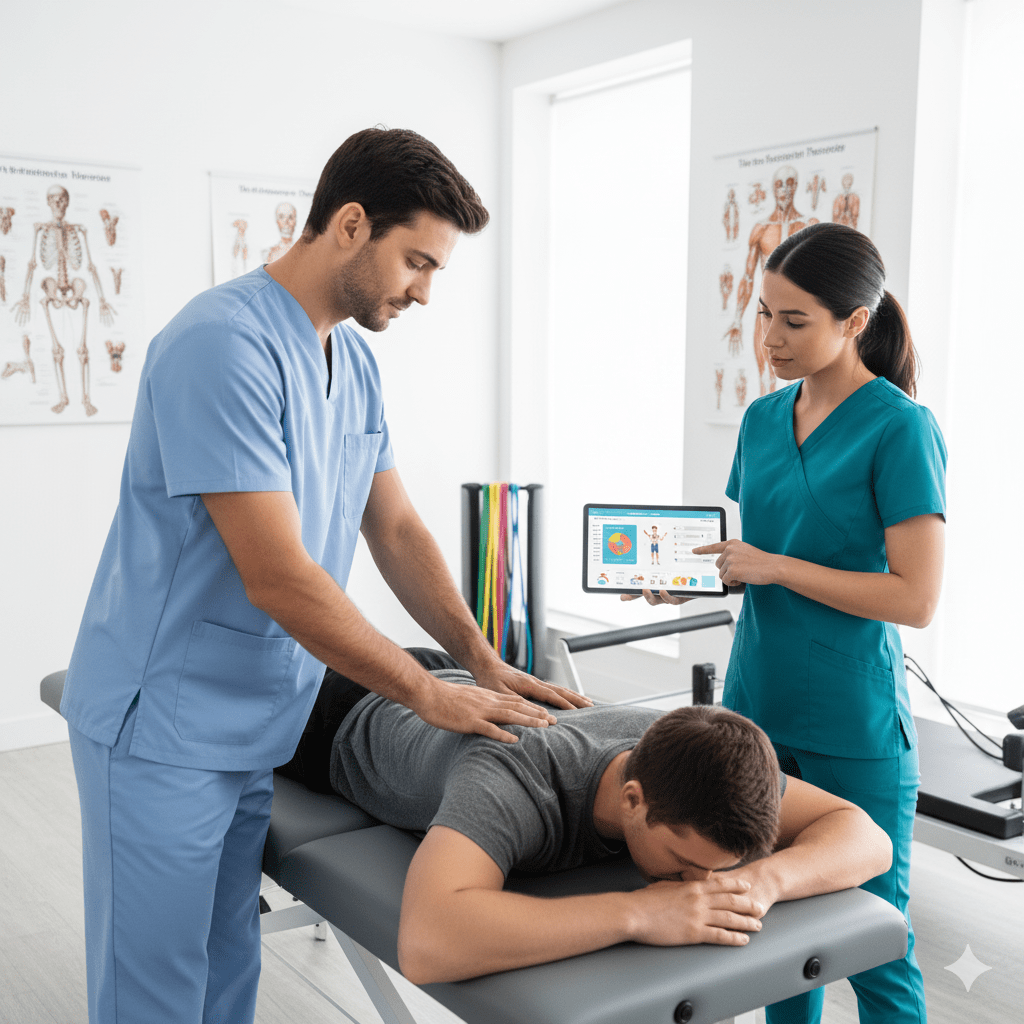
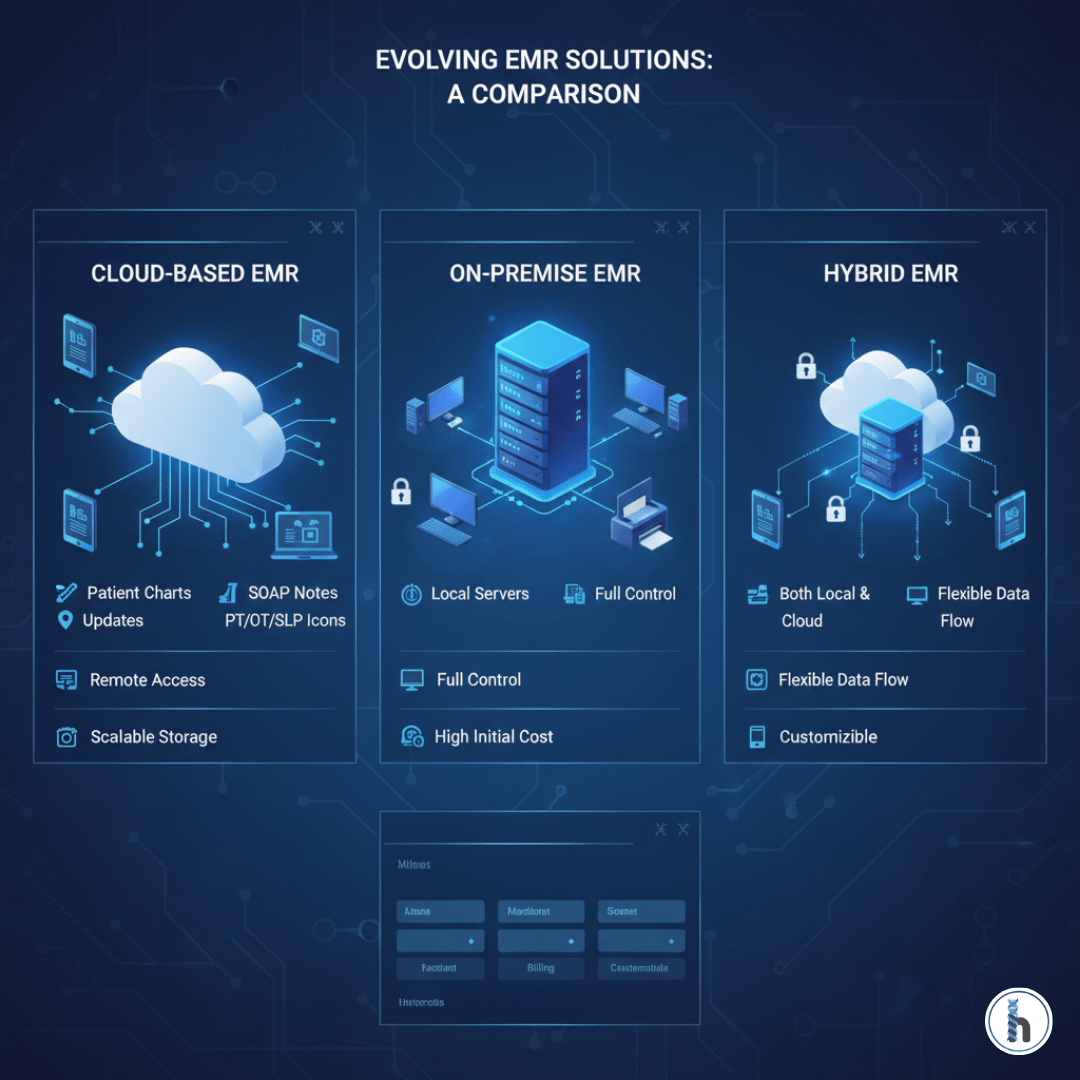
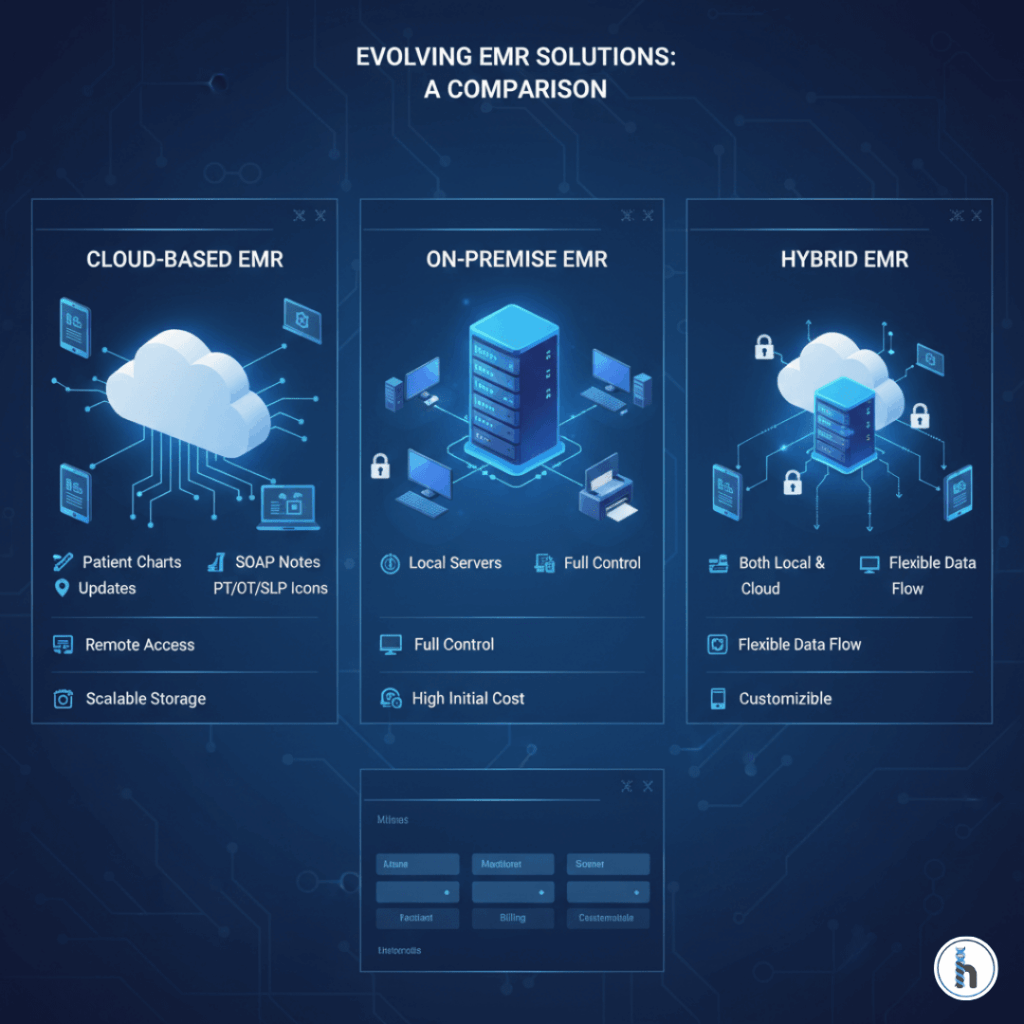
Bridging Academia and Clinic: The Role of EMR Solutions
The transition from a DPT program to clinical practice can be challenging, especially regarding documentation. This is where Electronic Medical Records (EMR) systems like HelloNote become essential.
HelloNote EMR is tailored for PTs, helping ease this transition by:
Streamlining evaluation documentation with intuitive templates.
Facilitating effective goal setting and tracking.
Simplifying billing and CPT code selection (e.g., 97110, 97112, 97140).
Enhancing compliance with built-in regulatory checks.
By reducing charting time, an EMR empowers new PTs to focus on patient care and skill development.
Conclusion: Preparing for a Rewarding Career
The path to becoming a physical therapist is demanding, but the framework is clear: complete a bachelor’s degree with the right prerequisites, graduate from a CAPTE-accredited DPT program, pass the NPTE, and obtain state licensure. For new graduates entering the field, leveraging tools like HelloNote EMR can significantly ease the transition, allowing them to focus on honing their clinical skills and making a meaningful impact on their patients’ lives from day one.
Frequently Asked Questions About How to Become a Physical Therapist
It typically takes about 7 years after high school. This includes a 4-year bachelor’s degree followed by a 3-year Doctor of Physical Therapy (DPT) program.
The entry-level degree required to practice as a physical therapist in the United States is the Doctor of Physical Therapy (DPT) from a program accredited by CAPTE.
The NPTE is the National Physical Therapy Examination. It is a standardized exam that all DPT graduates must pass to become licensed physical therapists. It assesses the essential knowledge and skills required for safe and effective entry-level practice.
No, a residency is not required to practice as a licensed physical therapist. Residencies are optional post-professional programs designed for PTs who wish to gain advanced expertise and specialize in a specific area like orthopedics, sports, or neurology.
An EMR like HelloNote helps new graduates by providing a structured framework for documentation that ensures compliance and accuracy. It simplifies goal tracking, helps with correct billing codes, and reduces administrative time, allowing new PTs to build confidence and focus on patient care.