What Telehealth Rules Will Actually Look Like for Therapy Clinics in 2026
Table of Contents
Telehealth has gone through more changes in the past few years than most therapy clinics expected. Temporary waivers, pandemic-era flexibilities, and shifting Medicare policies made it possible to deliver care remotely in ways that were once unthinkable.
As we move closer to Telehealth 2026, many therapy practice owners are asking the same questions:
What stays? What goes away? And what do we actually need to prepare for?
This article breaks down the most important telehealth updates affecting physical therapy, occupational therapy, speech-language pathology, and multidisciplinary rehab clinics without legal jargon or unnecessary speculation.

Why Telehealth Rules Matter More Than Ever
Telehealth is no longer an “extra” service. For many clinics, it’s become a core part of access, continuity of care, and patient engagement.
But the reality is this: telehealth is governed by policy, not preference. Reimbursement, compliance, and documentation rules determine what clinics can safely and sustainably offer.
As regulatory flexibility tightens, clinics that understand the rules early will be in a much stronger position than those reacting after denials or audits appear.
What’s Changing With Telehealth in 2026
Medicare Location Requirements Are Tightening
Through January 30, 2026, Medicare beneficiaries can generally receive telehealth services regardless of geographic location. After that date, most non–behavioral health telehealth services will once again be tied to rural locations and approved medical facilities.
This means:
Home-based telehealth will become more limited for certain services
Clinics must be precise about where the patient is located
Documentation must clearly support eligibility
Behavioral health services remain an important exception, with more flexibility continuing beyond early 2026.
Who Can Furnish Telehealth Services Is Narrowing
During the extended flexibility period, a wide range of providers were allowed to furnish telehealth services under Medicare.
Starting January 31, 2026:
will no longer be able to independently furnish Medicare telehealth services under standard Medicare rules.
This change is significant for therapy clinics that relied heavily on remote sessions and hybrid care models.
What This Means for Therapy Clinics
Telehealth Won’t Disappear But It Will Be More Regulated
Telehealth in 2026 is not about elimination it’s about precision.
Clinics will need to:
Clearly identify which services remain eligible
Track patient location accurately
Distinguish Medicare rules from commercial payer policies
Avoid assumptions based on past flexibilities
Documentation Will Matter More Than Ever
When telehealth rules tighten, documentation becomes your first line of defense.
Strong documentation should clearly show:
Medical necessity
Service type and duration
Patient location
Provider eligibility
Compliance with payer-specific rules
This is where many clinics struggle not clinically, but operationally.
Audio-Only Telehealth: What Still Applies
Audio-only telehealth services may continue for certain behavioral health services, particularly when:
The provider is capable of video
The patient cannot or does not consent to video
Documentation supports the clinical appropriateness
However, audio-only is not a blanket substitute for video-based care and must be used carefully.
Place of Service Codes Clinics Need to Know
Accurate coding remains critical for reimbursement.
Medicare continues to pay non-facility rates for telehealth services provided in the patient’s home, making correct POS selection essential.
How Technology Can Reduce Telehealth Risk
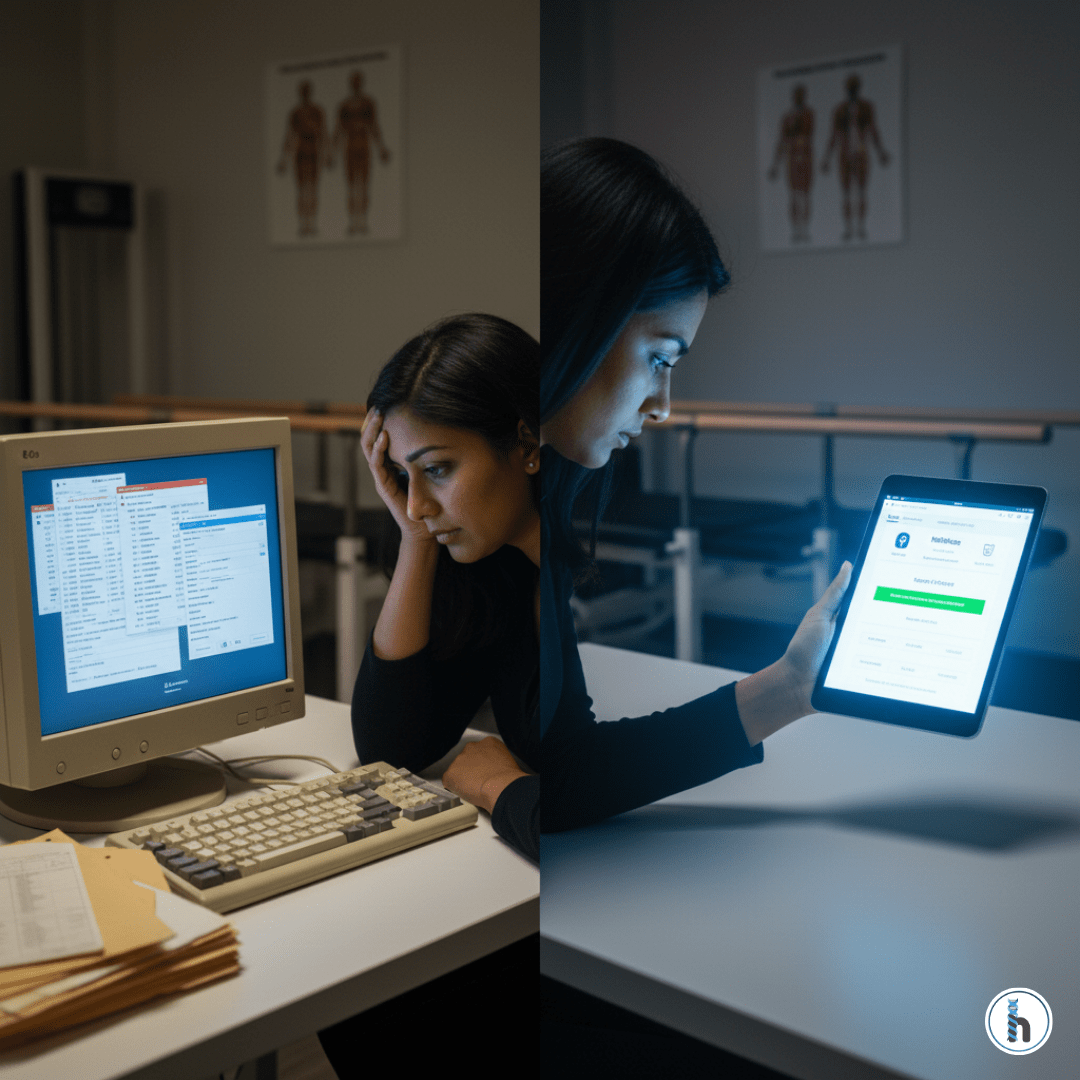
EMRs Must Do More Than Store Notes
As telehealth rules evolve, clinics need systems that actively support compliance not just record visits.
An effective EMR should help clinics:
Track patient location automatically
Prompt correct place of service selection
Align documentation with billing rules
Generate audit-ready records
Flag eligibility issues before claims are submitted
Without this support, telehealth becomes a financial and compliance liability.
Preparing Your Clinic for Telehealth 2026
Step 1: Audit Your Current Telehealth Usage
Understand which services, payers, and patient populations you’re serving remotely.
Step 2: Separate Medicare From Commercial Payer Rules
Commercial payers may continue telehealth coverage even as Medicare rules change.
Step 3: Strengthen Documentation Standards
Ensure every telehealth visit clearly supports medical necessity and eligibility.
Step 4: Use Systems Built for Therapy Workflows
Generic EMRs often miss therapy-specific nuances. Therapy-focused systems help reduce risk as regulations evolve.
Final Thoughts: Telehealth Requires Strategy, Not Guesswork
Telehealth 2026 represents a shift from emergency flexibility to long-term structure. Clinics that treat telehealth as a regulated service rather than a convenience will be best positioned to adapt.
With the right workflows, documentation practices, and technology in place, therapy clinics can continue using telehealth responsibly, compliantly, and confidently without exposing themselves to unnecessary risk.
Frequently Asked Questions About Telehealth 2026
Yes, but with more restrictions—especially for Medicare patients and non–behavioral health services.
Clear documentation, correct coding, accurate patient location tracking, and payer-specific workflows are key.
Not necessarily. Commercial payer rules may differ and should be reviewed individually.
Yes. Behavioral health continues to have expanded flexibility beyond early 2026.
Clear documentation, correct coding, accurate patient location tracking, and payer-specific workflows are key.