The landscape of professional education is continually evolving, driven by technological advancements and the need for greater accessibility. Within the rehabilitation therapy fields, this evolution is particularly evident in the rise of online degree programs, including those for aspiring Speech-Language Pathologists. For clinic owners, administrators, and practicing therapists (SLPs, OTs, and PTs), understanding the nature, quality, and implications of these online speech therapy degree programs is increasingly important for hiring, collaboration, and appreciating the diverse pathways into the profession.
This article explores the world of online speech therapy degree programs, shedding light on their structure, accreditation, benefits, challenges, and how they are shaping the future SLP workforce.

The Emergence of Online SLP Education: More Than Just Convenience
While flexibility is a significant draw, the growth of speech language pathology masters online goes beyond mere convenience. These programs have emerged to meet several critical needs
Addressing Geographic Barriers
Prospective students in rural or underserved areas may not have access to a traditional brick-and-mortar university offering an SLP program. Online options remove this limitation.
Increasing Accessibility for Diverse Learners
Online programs can offer pathways for non-traditional students, career changers, or individuals with family or work commitments that make full-time, on-campus study challenging.
Leveraging Technology for Enhanced Learning
Modern educational technology allows for sophisticated online learning experiences, including virtual labs, interactive simulations, and robust communication platforms for student-faculty and peer-to-peer interaction.
Meeting Growing Workforce Demands for SLPs
The demand for SLPs continues to grow across various settings (schools, hospitals, private clinics, early intervention). This expansion driven by online speech therapy degree programs helps expand the pipeline of qualified professionals entering the field.
What Does an “Online” SLP Program Actually Entail?
When exploring online speech therapy degree programs, it’s crucial to understand that reputable options are not simply correspondence courses; understanding these components is key when researching how to become a speech therapist online through a quality program. They typically involve a combination of learning modalities:
Didactic Coursework: Asynchronous and Synchronous Learning
Foundational knowledge (anatomy, physiology, neuroscience, phonetics, language development, acoustics, etc.) and specialized courses (aphasia, dysphagia, voice disorders, child language disorders, fluency, etc.) are delivered online. This often involves recorded lectures, readings, assignments, online discussions, and exams. Learning can be asynchronous (students access materials and complete work on their own schedule within set deadlines) or synchronous (requiring students to log in for live online classes or discussions at specific times), or a blend of both.
Supervised Clinical Practicum: Real-World Experience
This is the cornerstone of SLP training and cannot be completed entirely online. Online programs facilitate and oversee the required clinical clock hours (typically supervised by ASHA-certified SLPs) in real-world settings.
Potential Campus Visits for Hybrid Programs
Some online programs are fully online for coursework, while others are “hybrid” and may require occasional visits to campus for intensive labs, specific training modules, or orientations.
Accreditation: The Undisputed Seal of Quality for Online Speech Therapy Degrees
Perhaps the most critical factor when considering online speech therapy degree programs, or even traditional ones, is accreditation by the Council on Academic Accreditation in Audiology and Speech-Language Pathology (CAA) of the American Speech-Language-Hearing Association (ASHA).
Why CAA Accreditation Matters for SLP Careers
Graduation from a CAA-accredited program is essential for eligibility to obtain the Certificate of Clinical Competence in Speech-Language Pathology (CCC-SLP) from ASHA, which is the gold standard credential in the field. It answers the common question, ‘are online speech therapy degrees legitimate?’ by ensuring they meet rigorous national standards. It is also a requirement for state licensure in almost all states.
Ensuring Program Standards and Graduate Preparedness
Accreditation signifies that the program meets rigorous standards for curriculum, faculty qualifications, clinical education, resources, and student outcomes. It assures students, employers, and the public that graduates are adequately prepared for entry-level practice.
Verifying Accreditation Status
Prospective students and employers should always verify the status of accredited online SLP programs directly through the ASHA CAA website. Reputable online programs prominently display their accreditation.
Navigating the Clinical Education Component in Online SLP Programs
A common question surrounding SLP online programs clinical hours and experiences is how they are managed. Accredited online programs have robust systems in place.
Coordinated Clinical Placement Support
Programs typically have dedicated clinical placement coordinators who work with students to secure appropriate practicum sites and qualified supervisors in or near the student’s community.
Gaining Experience in Diverse Settings
Students are required to gain experience across different age groups and disorder types, just as in traditional programs. Placements might be in schools, hospitals, skilled nursing facilities, private practices, or early intervention programs.
Upholding ASHA Supervision Standards
All clinical hours must be supervised by an ASHA-certified SLP who meets specific supervision requirements. The quality of supervision is paramount, regardless of the program’s delivery format.
Technology Integration in Clinical Supervision
While supervision is in-person, technology might be used for communication between the student, the university supervisor, and the on-site supervisor (e.g., video conferencing for check-ins).
Advantages of Online SLP Programs for Students and the Profession
Online speech therapy degree programs offer distinct benefits for both students and the wider profession.
Unparalleled Flexibility and Work-Life Balance
Allows students to better balance education with work, family, or other obligations.
Enhanced Accessibility to SLP Education
Opens doors for individuals who cannot relocate or commute to a traditional campus.
Diverse Cohorts and Enriched Learning
Can bring together students from various geographic locations and backgrounds, enriching discussions and perspectives.
Innate Technology Proficiency for Modern Practice<
Graduates are often inherently comfortable with digital tools, communication platforms, and potentially telehealth technologies (like telehealth speech therapy), skills valuable in modern practice.
Potential Challenges and Considerations for Online SLP Students
Despite the advantages, there are considerations.
The Need for Self-Discipline and Time Management
Online learning requires significant motivation, time management, and organizational skills.
Essential Technology Requirements and Access
Reliable internet access and comfort with learning technologies are essential.
Securing Local Clinical Placements
Depending on the student’s location and the program’s network, securing suitable local placements can sometimes be challenging, requiring proactivity from both the student and the program.
Building a Strong Sense of Community Online
Creating a strong cohort connection can require more deliberate effort compared to on-campus programs. Programs often address this through virtual social events, group projects, and active discussion forums.
Understanding State Licensure Variations
While ASHA CCC-SLP requirements are national, specific state licensure rules can vary. Students must ensure their chosen program meets the requirements of the state(s) where they intend to practice.
Implications for Clinic Owners and Administrators Hiring Online Program Graduates
As graduates from online speech therapy degree programs enter the workforce, clinic owners and administrators should.
Focus on Competency, Not Program Format
Evaluate candidates based on their clinical skills, knowledge, critical thinking, and professionalism, just as you would graduates from traditional programs. The accreditation ensures they have met the required educational and clinical standards.
Recognize Potential Strengths of Online Graduates
Graduates may bring strong technology skills and adaptability.
Always Verify Credentials (Accreditation and Licensure)
Always confirm graduation from a CAA-accredited program and relevant state licensure.
Provide Robust Clinical Fellowship (CF) Support
Provide robust mentorship and supervision during the Clinical Fellowship (CF) year, regardless of the graduate’s educational pathway.
Streamlining Practice for Every Therapist: The Role of Technology and EMRs
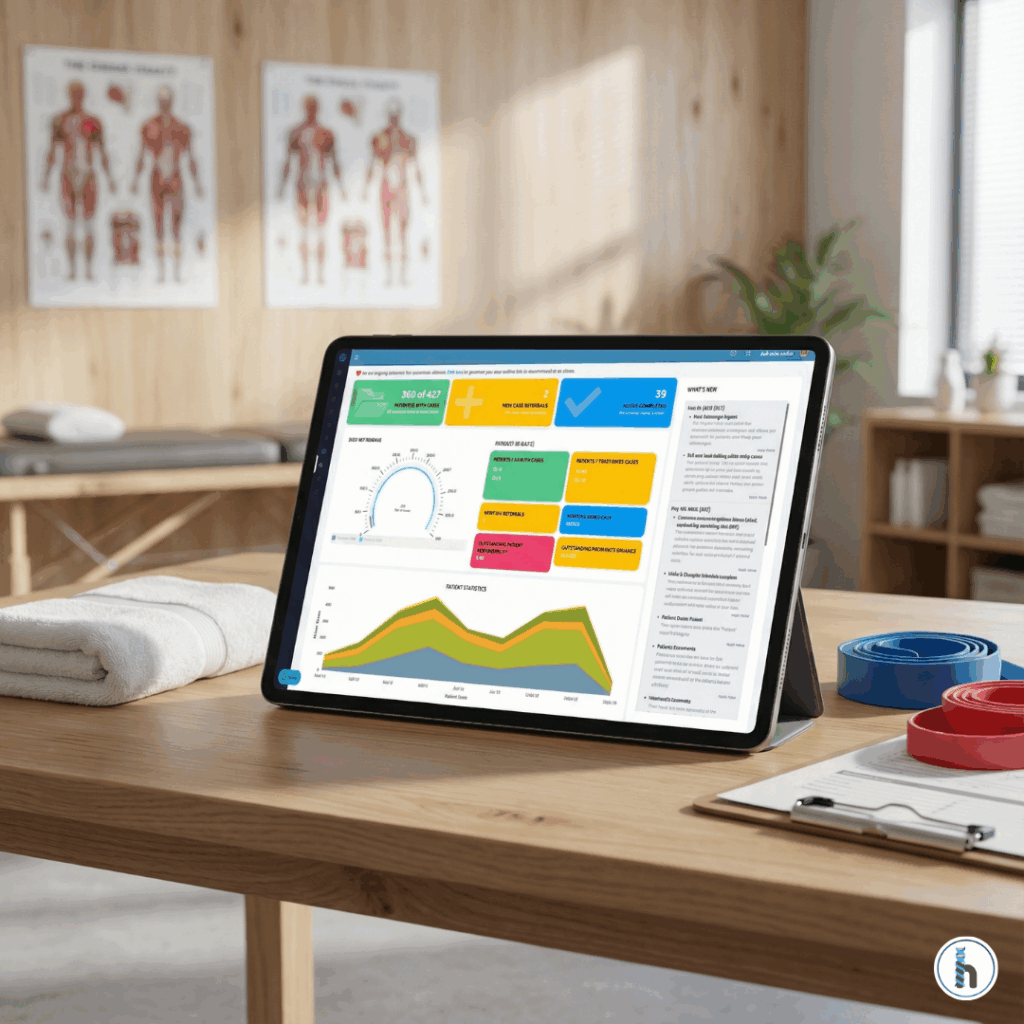
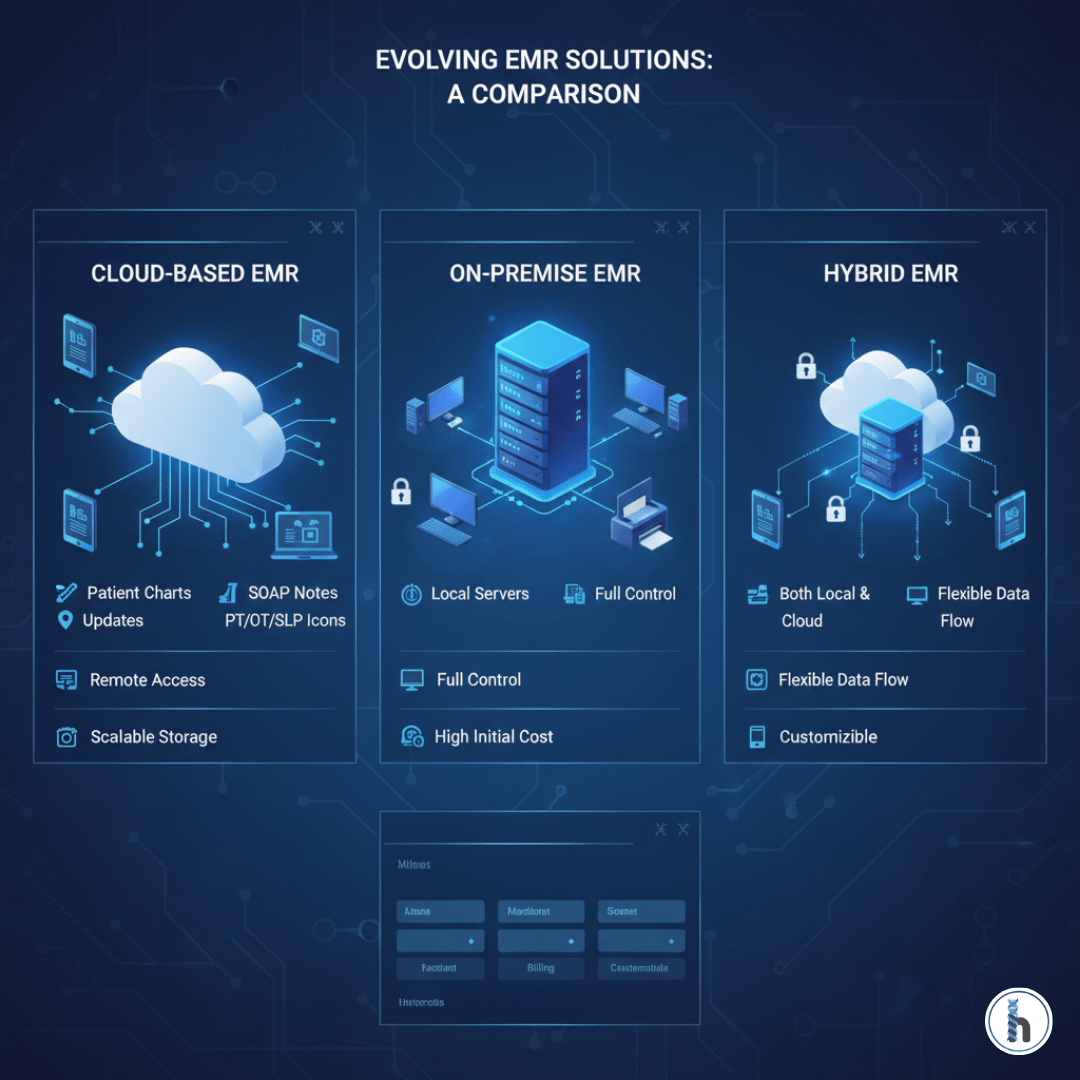
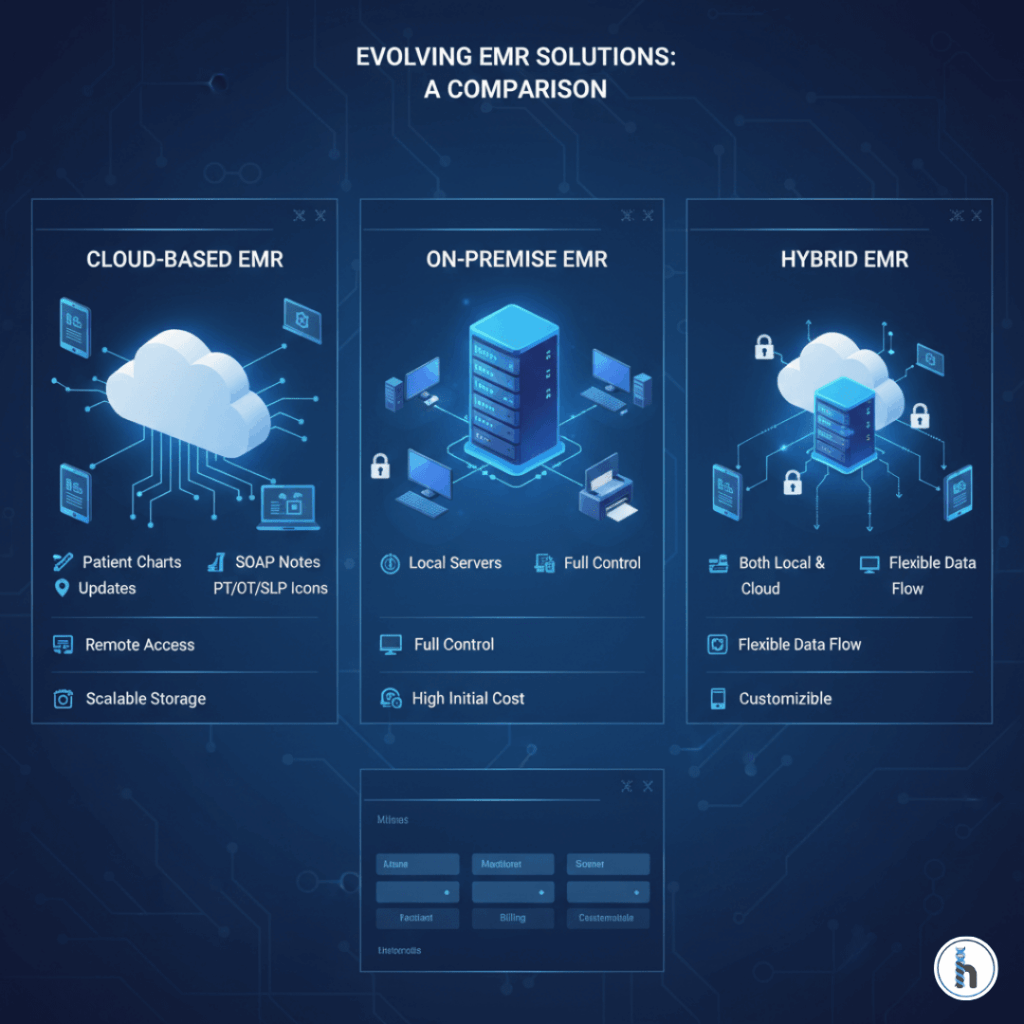
The rise of online education underscores the integral role technology plays in modern healthcare. Whether an SLP graduated from an online or a traditional program, efficiency, organization, and secure communication are vital for effective practice. This efficiency is paramount, whether one trained via an online SLP program or traditional campus, highlighting the need for robust SLP documentation software. This is where robust Electronic Medical Record (EMR) systems become indispensable tools for therapists and clinics.
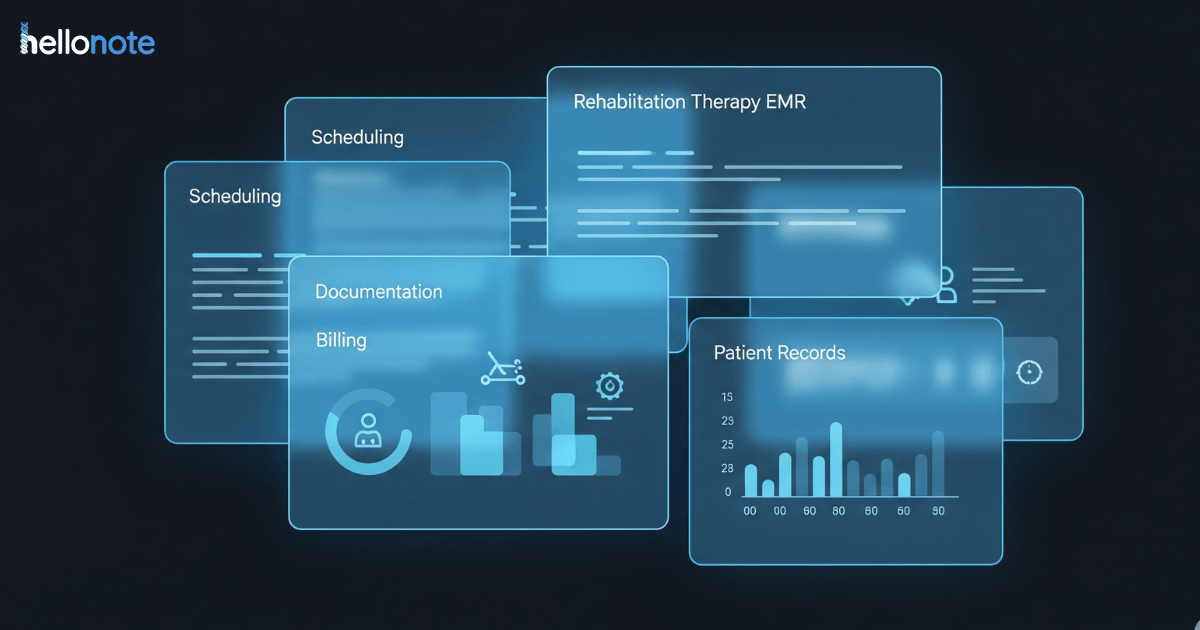
For SLPs, managing diverse caseloads, tracking complex goals, generating detailed documentation, and ensuring compliant billing requires significant administrative effort. An intuitive and therapy-specific EMR can dramatically reduce this burden, freeing up valuable time for direct patient care.
>How HelloNote Empowers SLPs and Therapy Clinics
HelloNote is a leading therapy EMR platform, specifically an EMR for SLPs, designed for the unique needs of rehabilitation therapists, including SLPs. It recognizes the unique workflow and documentation requirements of the profession, offering features that align perfectly with the need for efficiency and compliance highlighted by the integration of technology in both education and practice.
SLP-Specific Templates for Efficient Documentation
Utilize customizable templates for evaluations, treatment notes (SOAP notes), progress reports, and discharge summaries, tailored to various disorders and settings. This speeds up documentation while ensuring thoroughness.
Intuitive Goal Tracking and Progress Reporting
Easily create, track, and update patient goals, linking them directly to interventions and progress data within notes. This simplifies progress reporting and demonstrates treatment efficacy.
Integrated Billing for Improved Revenue Cycle<
Streamline the billing process with features that help ensure accuracy and compliance, reducing claim denials and improving revenue cycle management – a crucial aspect for clinic owners and administrators.
Secure Communication for Enhanced Team Collaboration
Facilitate secure messaging within the platform for better team collaboration and coordination of care, essential in multi-disciplinary clinics.
Cloud-Based Accessibility for Modern Therapists
As a cloud-based platform, HelloNote allows therapists and administrators secure access to patient information from anywhere, mirroring the flexibility valued in modern work and educational environments. By adopting a system like HelloNote, clinics can support all their therapists – regardless of their educational background – in working more efficiently, maintaining high standards of documentation, and ultimately focusing more energy on delivering excellent patient outcomes.
Conclusion: Embracing the Evolution of SLP Education and Practice
Online speech therapy degree programs, when CAA-accredited, represent a legitimate and valuable pathway into the profession. They effectively prepare individuals seeking how to become a speech therapist online for the realities of the profession. They produce competent, qualified SLPs equipped to meet the demands of modern practice. For established professionals, clinic owners, and administrators, understanding these programs allows for informed hiring decisions and a better appreciation of the diverse educational backgrounds within the field. As technology continues to shape both how therapists are trained and how they practice, embracing tools that enhance efficiency and effectiveness, like specialized EMRs, becomes increasingly vital for success across the rehabilitation therapy landscape.
Ready to Streamline Your SLP Practice with HelloNote?
Explore our features specifically designed for Speech-Language Pathologists or request a personalized demo today to discover how technology can support your practice’s success.