10 Massage Advertisement Strategies to Fill Your Calendar in 2026
Table of Contents
Introduction
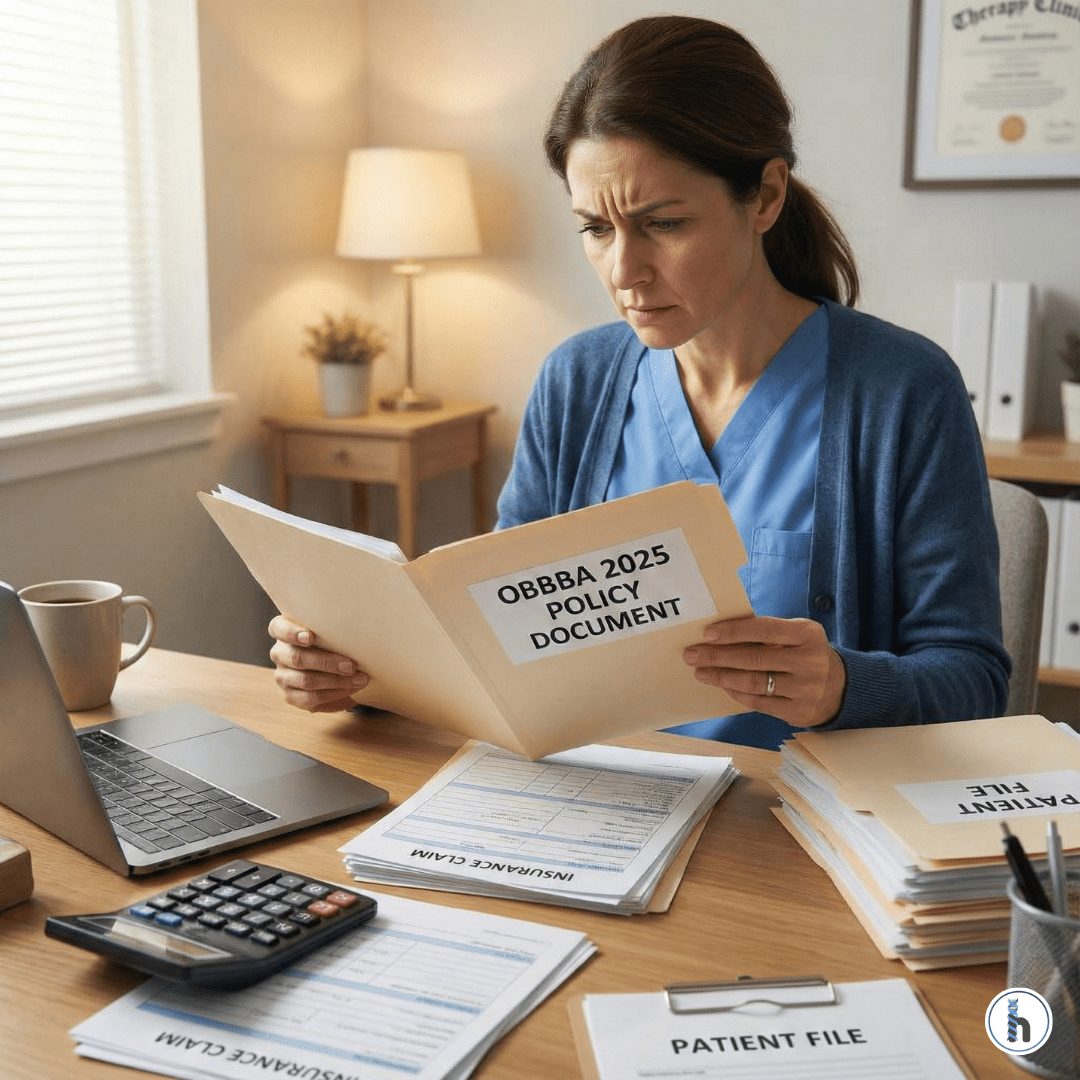
To consistently fill a massage calendar, advertisements must evolve beyond selling “luxury” and instead sell clinical outcomes combined with friction-free booking. When you target specific pain points, use social proof responsibly, and connect ads directly to seamless online scheduling through HelloNote, you convert high-intent searches into confirmed appointments. Marketing should not create administrative chaos; it should create predictable growth. This guide explores how to balance clinical authority with modern digital automation to build a sustainable, scalable practice.
The 2026 Massage Growth Blueprint
- Symptom-Specific Ads: Campaigns targeting “Tech Neck” or “Chronic Shoulder Tension” convert 3x better than general relaxation ads.
- AEO Dominance: AI search engines now prioritize “direct answers.” Use the FAQs at the bottom of this guide to capture this traffic.
- Friction-Free Booking: Every ad must link directly to HelloNote Online Booking to prevent lead drop-off.
- Retention Focus: Shift from selling visits at the front desk to documenting a Plan of Care in the treatment room.
Strategy Comparison: Impact vs. Effort
Strategy | Primary Goal | Effort Level | HelloNote Integration |
Google Local Search | Capture “Ready-to-Book” clients | High (initial setup) | Direct link to Online Booking |
Introductory Offers | Reduce entry barrier | Low | Automated First-Visit Discount Codes |
Symptom-Specific Ads | Establish clinical authority | Medium | Custom intake forms for specific pain |
Flash Sale (SMS/Email) | Fill last-minute cancellations | Very Low | Integrated Email/SMS marketing |
Clinical Marketing and HIPAA Compliance
Sanctuary Aesthetics vs. Clinical Authority
Visuals of candlelight and warm towels attract attention, but authority converts. When advertising symptom-specific relief—such as myofascial release for neck tension or manual therapy for postural strain—reference measurable outcomes like:
- Increased Range of Motion (ROM)
- Reduced pain scale (e.g., 8/10 to 3/10)
- Improved functional movement
HIPAA-Compliant Marketing
Growth without compliance creates risk. Testimonials are powerful, but written marketing releases are required before sharing identifiable patient details. Using a centralized system like HelloNote ensures marketing consents are stored alongside clinical records—protecting both your growth and your legal standing
10 Massage Advertisement Strategies That Actually Convert
1. Google Local Search Ads
Target high-intent searches like “massage near me” or “deep tissue massage [City].” These clients are solution-focused and ready to book immediately.
2. Symptom-Specific “Pain Point” Ads
“Dealing with Tech Neck?” targeted ads convert better than general wellness. Create a custom intake form in HelloNote for these specific pain-point clients to streamline their first visit.
3. The Introductory Offer
A first-visit discount lowers resistance. Use HelloNote to automate “First Visit” codes and ensure these new leads are placed into a retention-focused follow-up sequence.
4. The Visual Sanctuary Ad
High-quality images of your treatment space build trust. Clients want reassurance that your environment is clean, professional, and relaxing.
5. Testimonial & Social Proof Ads
Instead of “It was great,” use: “After three sessions, my migraine frequency dropped significantly.” (Always secure written consent first).
6. Seasonal Gift Card Campaigns
Mother’s Day, Valentine’s Day, and the Holidays are prime times for gift cards. Offer digital versions and embed the links into automated email campaigns.
7. Video “Meet the Therapist” Ads
Massage is personal. A 30–60 second introduction video builds a sense of safety and professional connection before the booking is ever made.
8. The “Self-Care as Maintenance” Campaign
Shift the narrative from luxury to necessity. This supports recurring bookings and membership models, which provide more stable revenue.
9. Referral Program Promotion
Track referral sources inside HelloNote to reward your most powerful marketing channel: your current happy clients.
10. Last-Minute Opening Flash Sale
Cancellation at 2:00 PM? Send an SMS blast through HelloNote offering a complimentary upgrade. Scarcity and immediacy fill schedule gaps in minutes.

The Therapist’s Insight: From Booking to Re-Booking
In my experience running a busy practice, the biggest issue isn’t lead generation—it’s retention. The mistake many make is trying to sell the next visit at the front desk. Instead, sell the Plan of Care in the treatment room. Document “Recommended Frequency” directly in the HelloNote Assessment section while the client is still on the table. This feels clinical and supportive, not sales driven.
Frequently Asked Questions
Require a credit card on file or a deposit during online booking. HelloNote’s Fiserv integration makes this seamless. Clinics requiring deposits typically see a 65% reduction in ghosting and last-minute cancellations.
For 2026, the highest-converting “high-intent” keywords are “massage for back pain [City],” “deep tissue massage near me,” and “sports massage for [Specific Injury].”
Create a custom Referral Source in your HelloNote EMR labeled “Instagram – Tech Neck.” Assign new clients accordingly and run a monthly Referral Report to see exactly how much revenue that campaign generated.
Yes. Filter your client list by birth month in your EMR and send automated email promotions containing a digital gift card link. This is one of the most effective ways to fill mid-week schedule gaps.
Yes, as long as you have a signed HIPAA-compliant marketing release on file. It is best practice to use first name and last initial only to maintain a high standard of patient privacy.