2026 RTM Code Update: What Therapy Clinics Need to Know About 98985 & 98979
Table of Contents
As of January 1, 2026, Medicare has implemented important updates to Remote Therapeutic Monitoring (RTM) billing that directly affect physical therapy, occupational therapy, and speech-language pathology practices.
These updates introduce new HCPCS codes and revise existing ones, changing how clinics document, bill, and get paid for RTM services. For therapy clinics using digital monitoring tools, home exercise tracking, or hybrid care models, these changes are not optional—they directly impact reimbursement, compliance, and audit risk.
This guide breaks down:
- What changed in the 2026 RTM code update
- How codes 98985 and 98979 are used
- What Medicare expects from therapy documentation
- Common billing pitfalls to avoid
- How clinics can operationalize RTM correctly in 2026
What Changed in the 2026 RTM Code Update
In late 2025, CMS released Transmittal 13431, updating the Medicare Therapy Code List and expanding RTM-related billing options.
New and Updated RTM Codes for 2026
Medicare now recognizes the following RTM-related HCPCS codes as “Sometimes Therapy” services when billed by therapists:
- 98985 – RTM device supply for musculoskeletal monitoring, 2–15 days in a 30-day period
- 98984 – RTM device supply for respiratory monitoring, 2–15 days
- 98979 – RTM treatment management services, first 10 minutes per calendar month
In addition, existing codes were updated:
- 98976 / 98977 now cover 16–30 days of monitoring instead of shorter periods
Why “Sometimes Therapy” Classification Matters
When therapists bill these RTM codes, Medicare requires:
- An active therapy plan of care
- The correct discipline-specific modifier
- GP for PT
- GO for OT
- GN for SLP
- Documentation that clearly ties RTM services to skilled therapy intervention
Failure to meet these conditions can result in denials or post-payment audits.
Why the 2026 RTM Update Matters for Therapy Clinics
Clinics that fail to adapt to the 2026 update may face:
- Claim denials due to invalid or outdated codes
- Lost revenue from uncompensated services
- Compliance exposure from missing modifiers or unsupported documentation
Medicare is increasingly strict about RTM claims, especially when services overlap with traditional therapy visits.
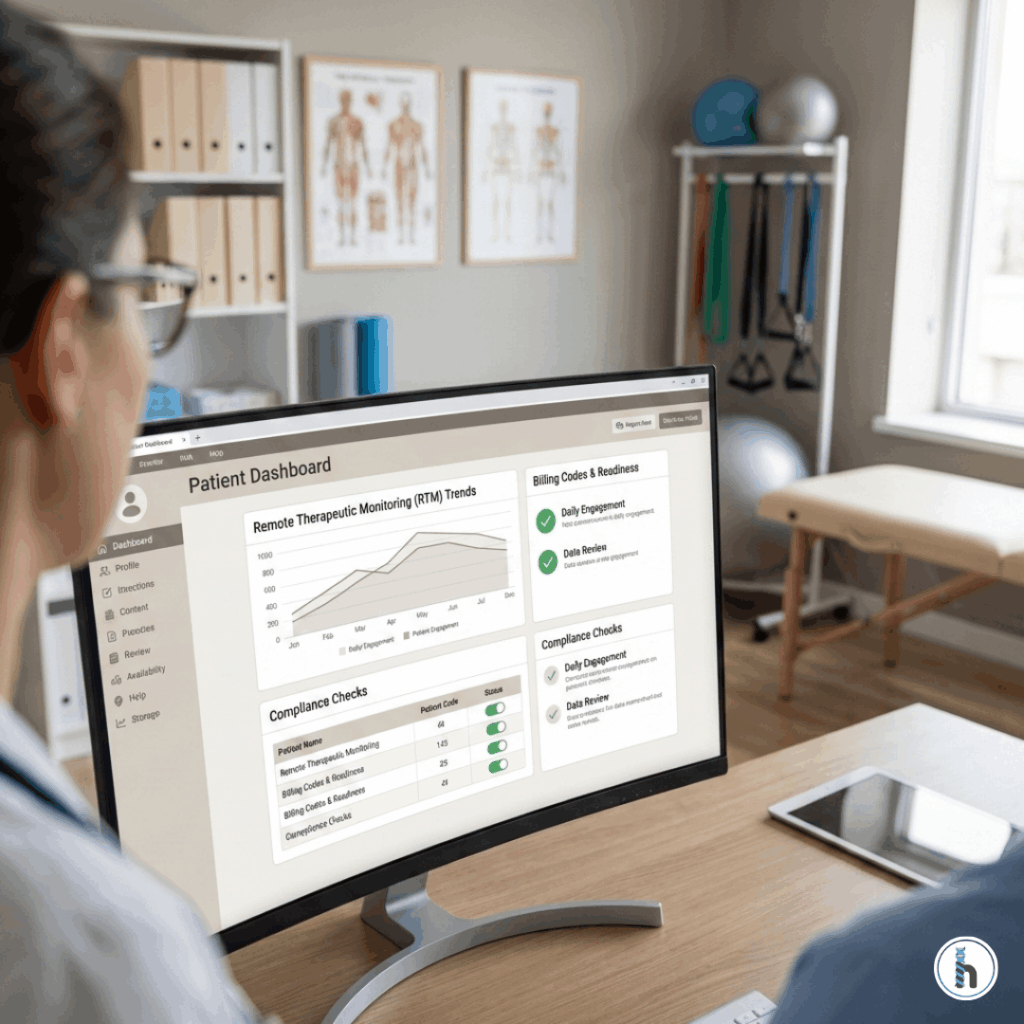
Documentation Expectations for RTM Billing in 2026
RTM services must be clearly distinguishable from routine therapy care.
What Medicare Expects to See in RTM Documentation
To support codes like 98985 and 98979, documentation should include:
- Evidence of device-based monitoring
- Clear linkage to the therapy plan of care
- Description of data reviewed (adherence, performance, trends)
- Therapist interpretation and clinical decision-making
- Time spent on RTM treatment management (for 98979)
RTM documentation should demonstrate skilled oversight, not passive data collection.
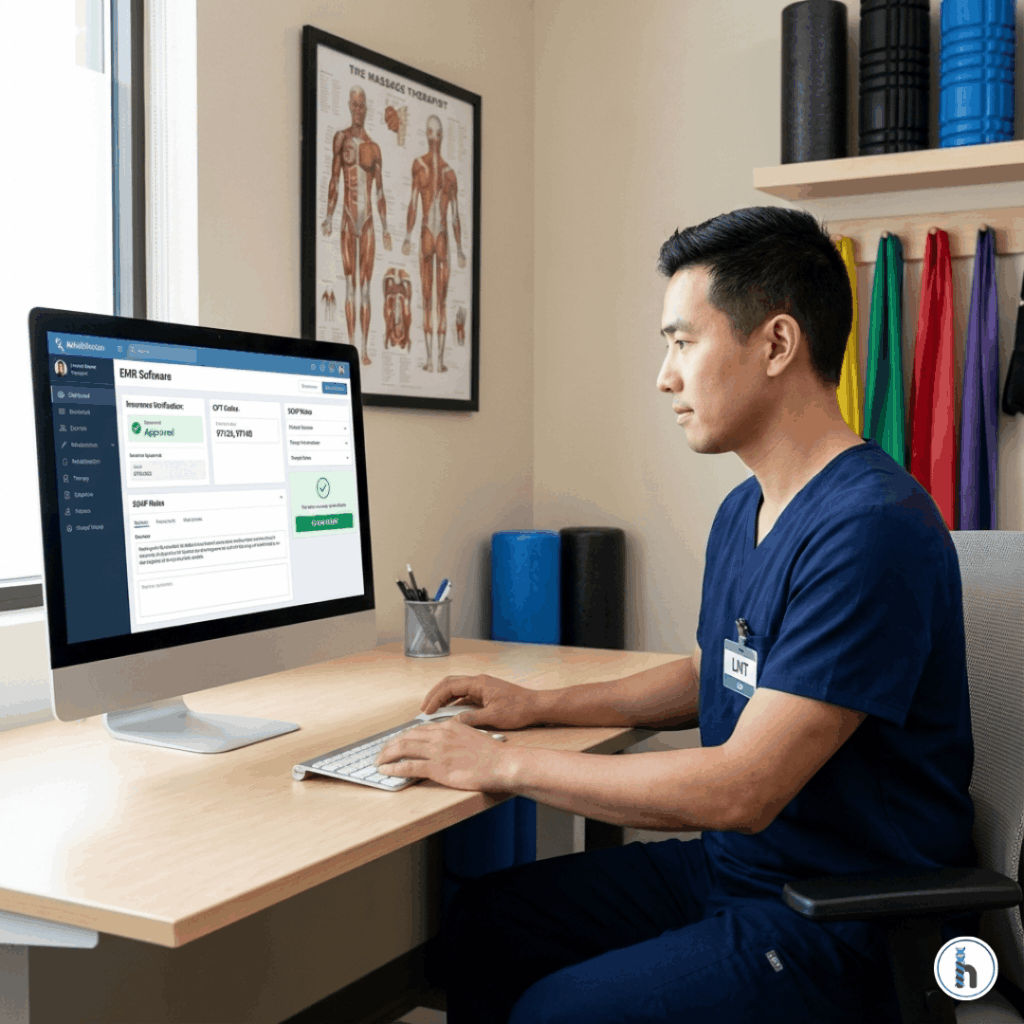
Modifier Requirements for RTM Codes
Correct modifier usage is critical.
RTM Modifier Summary for Therapy Clinics
Code | Description | Required Modifier |
98985 | MSK RTM device supply (2–15 days) | GP / GO / GN |
98979 | RTM treatment management (first 10 mins) | GP / GO / GN |
98976 / 98977 | RTM device supply (16–30 days) | GP / GO / GN |
CQ / CO | Assistant involvement | Only when applicable |
Missing or incorrect modifiers remain one of the top RTM denial triggers.
Operational Steps Clinics Should Take Now
Even with system support, clinics must align workflows.
1. Educate Clinical and Billing Teams
Ensure therapists understand:
- When RTM services qualify for billing
- Which codes apply to which scenarios
- How documentation supports reimbursement
2. Review RTM Workflows
Confirm that:
- RTM services are triggered intentionally
- Goals and outcomes are clearly documented
- Time-based services are tracked accurately
3. Monitor Early 2026 Claims
During the first quarter of 2026:
- Track RTM claim approval rates
- Identify denial patterns early
- Adjust documentation or modifier use if needed
Example RTM Billing Workflow (PT Scenario)
A physical therapist monitors a patient’s home exercise compliance using a digital MSK device:
- The therapist assigns RTM monitoring for 10 days
- RTM data is reviewed and interpreted within the therapy plan
- 98985 (GP modifier) is billed for device monitoring
- At month’s end, the therapist spends 10 minutes reviewing trends and adjusting care
- 98979 (GP modifier) is billed for RTM treatment management
When documented and billed correctly, this workflow supports clean claims and compliant reimbursement.
Frequently Asked Questions (FAQ)
Remote Therapeutic Monitoring (RTM) allows therapists to bill for monitoring patient data collected via approved devices between visits, when tied to a therapy plan of care.
The key additions are 98985 (MSK device supply, 2–15 days) and 98979 (RTM treatment management, first 10 minutes).
Yes, when RTM services are part of an active therapy plan of care and billed with the correct discipline-specific modifier.
Yes. Time must be documented for treatment management services like 98979.
The most common issues are missing modifiers, weak documentation linking RTM to skilled therapy, and using outdated codes.
Final Takeaway for 2026
The 2026 RTM update is not a minor coding change—it represents Medicare’s continued shift toward digitally supported therapy care.
Clinics that adapt early will benefit from:
- Expanded reimbursable services
- Stronger continuity of care
- Reduced billing friction
Clinics that delay risk denials, audits, and unnecessary revenue loss.