Understanding Your EMR System: Databases, Security, and Function
An EMR system (Electronic Medical Record system) is central to modern healthcare, transforming how providers document, access, and share patient information. At its core lies a structured database designed to securely manage vast amounts of clinical and administrative data. For therapy practices, understanding this digital infrastructure is critical for accurate documentation, efficient billing, and ensuring compliance with data protection regulations like HIPAA.
Despite their central role in daily operations, the underlying databases within these platforms are often misunderstood. What exactly do they store? How are they structured? And most importantly, how does the overall software protect sensitive patient information?
This article explores the function and structure of the EMR system, focusing on its core database component and how it serves physical, occupational, and speech therapy professionals. From its technical foundation and security protocols to integration capabilities, understanding this technology can help therapy clinics make informed decisions about their digital infrastructure and safeguard the trust placed in them by their patients.
What is an EMR System?
An Electronic Medical Record system is a digital platform used by clinicians to create, store, manage, and track patient health information electronically. It replaces traditional paper charts and provides a centralized hub for all clinical and administrative data. The EMR database is the core component within this platform that handles the actual storage and organization of information.
In therapy practices, such a system typically manages:
-
-
Patient demographics and medical history
-
Therapy notes, evaluations, and standardized test results
-
Progress reports and detailed care plans
-
Billing records, superbills, and insurance information
-
Appointment scheduling and communication logs
-
EMR Technology vs. Traditional Paper Records
Paper records have long been the standard, but their limitations compared to modern electronic records are significant:
-
-
Prone to physical degradation, loss, or destruction
-
Difficult to duplicate, share quickly, or access remotely
-
Time-consuming for filing, retrieval, and updates
-
Susceptible to illegibility and manual errors
-
By contrast, electronic record-keeping provides a secure, dynamic, and scalable alternative, offering key benefits for efficiency and compliance.
Core Components of an EMR’s Architecture
A well-designed electronic medical record architecture consists of several key components working together, centered around the database:
The EMR Database
The heart of the platform. It stores all structured patient data, including clinical notes, ICD/CPT codes, and billing history. As mentioned earlier, it often functions as a relational database.
Application Layer (User Interface)
This is what therapists interact with – the screens, forms, and workflows. It interfaces between the user and the database, enabling data entry, report generation, scheduling, and communication.
Security Layer (Ensuring Platform Security)
Crucial for HIPAA compliance. This includes role-based access controls, robust encryption protocols (for data at rest and in transit), and comprehensive audit trails to monitor data usage and access.
Integration Framework (Interoperability)
Allows the software to connect securely with external services such as billing software, patient portals, telehealth platforms, or clearinghouses, enabling seamless data exchange.
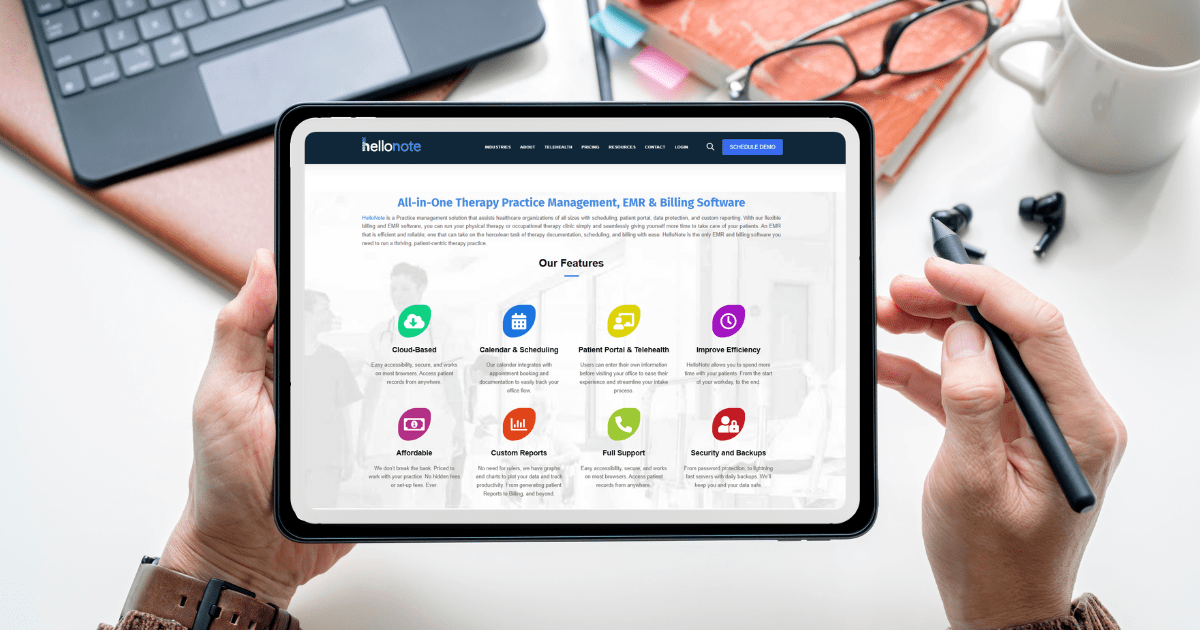
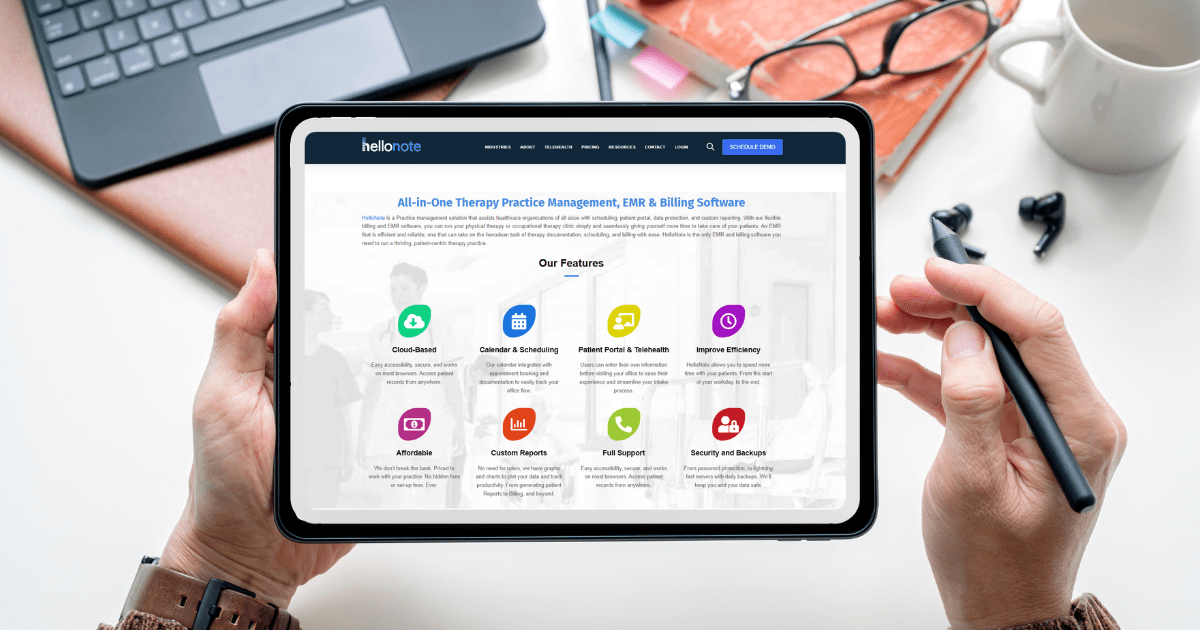
HelloNote, as a therapy-specific solution, integrates these components, offering customizable documentation, integrated billing, and secure cloud-based storage suitable for various practice sizes.
How EMR Platforms Protect Patient Information (Data Security)
One of the primary benefits of using electronic medical records is enhanced data security compared to paper. Safeguarding protected health information (PHI) is paramount. Modern healthcare platforms employ multi-layered security features:
1. Encryption at Rest and in Transit
Data within the database is encrypted both when stored and during transmission, making it unreadable without authorization.
2. Role-Based Access Control (RBAC)
Access to sensitive information is strictly limited based on user roles and permissions defined within the software.
3. Regular Backups and Redundancy
These systems perform frequent, automated backups, often stored in geographically separate, secure locations to prevent data loss.
4. Audit Trails for HIPAA Compliance
Detailed logs track all user activity (who accessed what, when), which is essential for accountability and meeting HIPAA requirements.
5. Secure Cloud-Based Advantages
Many modern solutions, including HelloNote, are cloud-based. This typically offers higher security standards maintained by specialized IT teams, better uptime, and faster disaster recovery compared to managing on-premise servers.
The Paramount Importance of PHI Security within Healthcare Technology
While digital platforms streamline workflows and improve data access, their most critical function is the secure protection of PHI. This is achieved through the robust security layers discussed above. Maintaining patient trust and ensuring HIPAA compliance hinges on the effectiveness of the platform’s security measures. This foundation enables all other benefits.
Common Challenges and How Robust EMR Software Addresses Them
Implementing or using electronic records can present challenges:
1. Integration with Existing Tools (Interoperability)
A strong platform supports API integration, allowing seamless data flow with other essential tools (billing, scheduling) without creating data silos.
2. Scalability for Practice Growth
Cloud-based solutions are inherently scalable, easily adapting to increased data volume, users, and locations without major infrastructure changes.
3. Data Migration and Onboarding
Reputable vendors offer tools and support for securely migrating data from old systems or paper records.
4. User Training and Data Entry Consistency
Well-designed software like HelloNote uses templates, required fields, and intuitive workflows to guide users, improving data quality and consistency.
The Future of EMR Technology in Therapy Practices
Electronic medical record technology will become even more central, supporting value-based care, patient engagement, and data analytics. Future therapy software features like predictive analytics, integrated remote patient monitoring, and AI-assisted documentation will rely heavily on the capabilities of the underlying platform and its database. Investing in a robust, secure solution prepares practices for these advancements.
Conclusion: Why Understanding Your Healthcare Technology Matters
Understanding the components, security measures, and capabilities of your chosen EMR system is essential for clinic owners and therapy professionals leveraging modern healthcare tools. It’s the foundation of efficient operations, quality care delivery, and regulatory compliance.
By providing secure, scalable, and increasingly interoperable platforms, these technologies reduce administrative burden, enhance clinical accuracy, and ensure your practice is future-ready. When evaluating solutions like HelloNote EMR, consider the entire architecture – user interface, database structure, security protocols, and integration potential – to find the best fit for your therapy practice.
Take the Next Step with HelloNote EMR
Looking to learn more about how a therapy-specific EMR can support your clinic’s growth? Explore HelloNote’s features and see how its platform can work for you.