Table of Contents
Choosing an electronic medical record is no longer just an IT decision it’s a clinical, operational, and financial one. For therapy practices, the wrong system doesn’t just slow things down. It adds documentation stress, creates billing risk, and pulls therapists away from patient care.
An electronic medical record for therapists should support how care is actually delivered not force clinicians to work around software limitations. Yet many practices still rely on platforms built for general medicine, not rehab-focused workflows.
This guide breaks down what therapists should realistically expect from an EMR and how to avoid costly mistakes when choosing one.
Why the EMR Decision Matters More for Therapy Practices
Therapy documentation is fundamentally different from primary care. Goals evolve session by session. Progress needs to be measurable. Billing depends heavily on time, modifiers, and medical necessity.
When an EMR isn’t designed for this reality, practices experience:
Longer documentation times after hours
Increased claim denials and delayed payments
Missed reassessments and compliance gaps
Burnout among clinicians and support staff
An effective EMR doesn’t just store notes it actively supports care delivery, compliance, and business health.
What Therapists Actually Need From an EMR
Not every feature advertised by EMR vendors matters. What does matter is how the system supports daily clinical and administrative work.
1. Therapy-Specific Documentation Workflows
Therapists need tools built around evaluations, daily notes, progress reports, and plans of care not generic SOAP notes.
A strong EMR should allow you to:
Link goals directly to daily treatment notes
Track objective progress over time
Reuse structured language without copy-paste errors
Complete notes efficiently during or immediately after sessions
When documentation mirrors clinical reasoning, notes become clearer and faster to complete.
2. Integrated Billing and Coding Supportc
Documentation and billing should not live in separate systems or separate mental processes.
A therapist-friendly EMR helps by:
Aligning CPT codes with documented services
Prompting for medical necessity where required
Supporting payer-specific rules and modifiers
Reducing manual rework between clinical and billing teams
This alignment is critical for protecting reimbursement and reducing audit risk.
3. Compliance Without Extra Work
Compliance shouldn’t rely on memory or sticky notes. The right system builds safeguards into the workflow.
Key compliance support includes:
Plan of care and progress note reminders
Time-stamped documentation trails
Secure patient communication tools
Audit-ready records without manual assembly
An electronic medical record for therapists should make compliance feel automatic—not stressful.
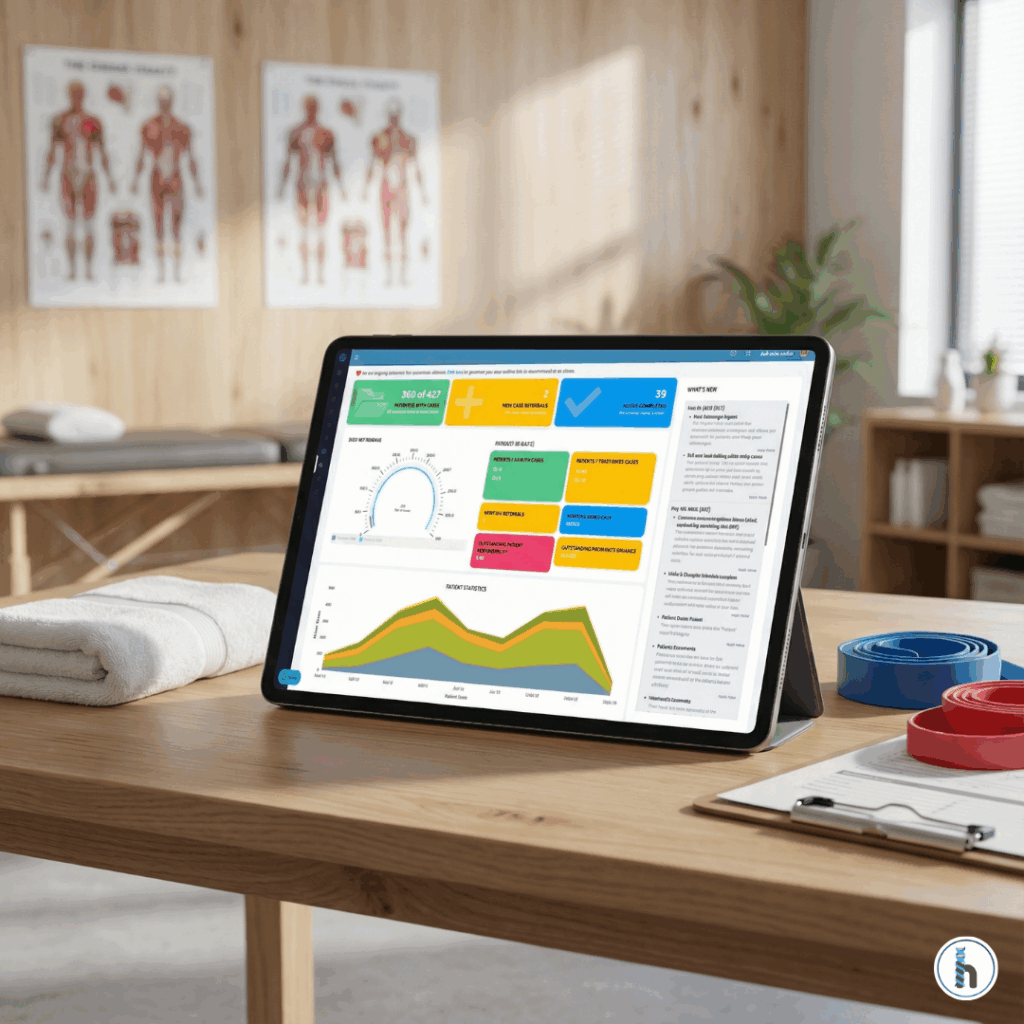
4. Visibility Across the Practice
Therapists, front desk staff, billers, and owners all rely on the EMR but for different reasons.
A well-designed system provides:
Clear dashboards showing what’s due or missing
Alerts for incomplete documentation or billing issues
Shared visibility without duplicated effort
When everyone works from the same system, fewer things fall through the cracks.
The Hidden Cost of the Wrong EMR
Many practices stay with outdated systems simply because switching feels risky. But the cost of staying is often higher.
Hidden costs include:
Lost clinician time spent correcting documentation
Revenue leakage from preventable denials
Higher staff turnover due to frustration
Limited ability to scale services or locations
Over time, these inefficiencies compound making growth harder and margins thinner.
How Modern EMRs Support Practice Growth
Today’s best EMRs are no longer passive record-keeping tools. They actively support smarter operations.
Modern platforms help practices:
Handle higher patient volume without adding staff
Launch new service lines confidently
Make data-informed business decisions
Improve therapist satisfaction and retention
This is where the EMR shifts from an expense to a strategic asset.
Making the Right Choice Without the Guesswork
When evaluating options, therapists should ask practical questions:
Does this system reflect how therapy is actually delivered?
Will it reduce time spent documenting not increase it?
Does it support billing accuracy and compliance by default?
Can it grow with the practice over time?
An electronic medical record for therapists should simplify work, not complicate it.
Final Thoughts
Therapists don’t need more software. They need better support for the work they already do every day.
The right EMR respects clinical judgment, protects reimbursement, and gives therapists their time back. When chosen thoughtfully, it becomes a foundation for better care, healthier teams, and sustainable growth.
If your current system feels like a barrier instead of a partner, it may be time to rethink what your EMR should actually be doing for you.
Frequently Asked Questions About Electronic Medical Records for Therapists
An electronic medical record for therapists is a digital system designed specifically to support physical therapy, occupational therapy, speech-language pathology, and other rehab disciplines. Unlike general medical EMRs, it focuses on therapy documentation, goal tracking, plans of care, and time-based billing workflows.
Therapy EMRs are built around functional outcomes, progressive goals, and frequent documentation updates. General medical EMRs are often visit-based and problem-focused, which can make therapy documentation slower and less intuitive.
Yes. Small practices often feel the impact of inefficient documentation and billing more quickly. A therapy-specific EMR helps reduce admin time, minimize claim errors, and keep workflows manageable without adding staff.
A well-designed EMR supports compliant documentation by linking services to goals, prompting for medical necessity, and aligning CPT codes with treatment notes. This reduces denials and makes audits easier to manage.
Practices should consider switching if documentation takes too long, billing errors are frequent, compliance feels stressful, or the system doesn’t support growth. These are signs the EMR is working against the practice instead of supporting it.