Therapy Scheduling Software That Improves Patient Flow
Table of Contents
In a therapy practice, scheduling isn’t just about filling time slots.
It’s about managing patient expectations, reducing no-shows, protecting staff time, and keeping the entire clinic aligned throughout the day.
HelloNote’s Scheduling & Patient Flow tools are built specifically for therapy clinics—supporting real-world workflows for physical therapy, occupational therapy, speech therapy, and multidisciplinary practices.
From the moment an appointment is booked to the moment a patient is discharged, HelloNote helps clinics stay organized, efficient, and patient-centered.
Customize Your Therapy Clinic Calendar to Match Your Workflow

No two therapy clinics operate the same way. Some need a tight daily view. Others plan weeks ahead across multiple providers.
HelloNote allows clinics to customize how many days appear in the schedule, making it easier to focus on what matters most—whether that’s today’s patient load or future availability.
Block Time to Protect Staff and Prevent Errors
Clinics can block time directly on the calendar for:
- Lunch breaks
- Team meetings
- Vacation days
- Administrative or documentation time
Blocked time appears clearly on the schedule, preventing double-booking and last-minute disruptions.
Why this matters:
Clear calendars reduce scheduling mistakes, staff burnout, and workflow interruptions—especially in busy outpatient clinics.
Offer Online Scheduling Through Your Therapy Website
Modern patients expect convenience. HelloNote makes it easy to offer online appointment scheduling through a secure Patient Portal link embedded directly on your clinic website.
Patients can book appointments without calling the front desk, while staff maintain full control over availability and appointment rules.
Why this matters:
Online scheduling reduces phone volume, captures appointments after hours, and improves the patient experience without increasing admin workload.
Automated Appointment Confirmations That Reduce Confusion
Once an appointment is scheduled, HelloNote automatically sends appointment confirmations via email and SMS.
These confirmations clearly communicate:
- Appointment date and time
- Location or clinic details
- Reassurance that the visit is booked
Why this matters:
Clear confirmations reduce cancellations caused by uncertainty and miscommunication.
Appointment Reminders That Reduce No-Shows
Missed appointments cost clinics time, revenue, and care continuity. HelloNote helps reduce no-shows with automated appointment reminders sent by email and SMS.
Clinics can:
- Enable reminders per patient
- Choose when reminders are sent (hours or days before visits)
- Use email, SMS, or both
- Include confirmation links when needed
If a patient accidentally unsubscribes, resubscribing is simple and quick.
Why this matters:
Consistent, automated reminders significantly reduce no-shows without adding extra work for your staff.
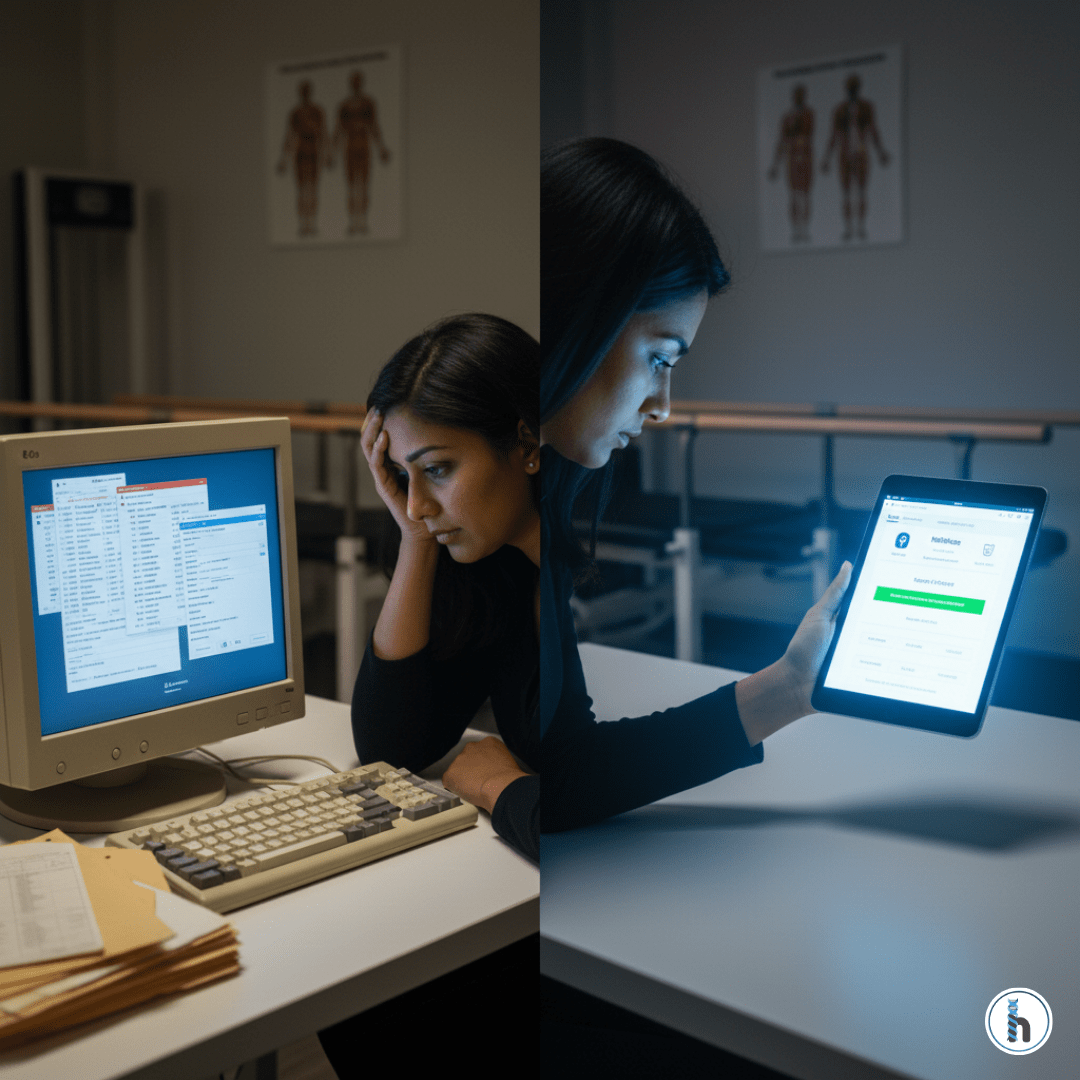
Internal Task and Event Reminders for Therapy Teams
Patient care doesn’t stop when a visit ends. Follow-ups, documentation, and administrative tasks all require coordination.
HelloNote supports internal reminders using two built-in tools:
Patient Alerts
Persistent notes attached directly to a patient’s chart—ideal for ongoing reminders or special instructions.
Event Reminders
Time-based reminders with due dates and notifications for tasks like authorizations, follow-ups, or discharge planning.
Why this matters:
Internal reminders help teams stay organized without relying on memory, sticky notes, or disconnected systems.
Real-Time Patient Status Tracking Across Your Clinic
Knowing where each patient stands—at a glance—improves coordination across front desk and clinical teams.
HelloNote’s Patient Status Tracker allows clinics to view and update patient statuses in real time, including:
- Active
- Evaluation
- Inactive
- Needs Authorization
- Needs Eligibility
- Needs Discharge
Statuses can be updated instantly using drag-and-drop functionality.
Why this matters:
Real-time visibility reduces delays, improves communication, and supports better operational decisions across the clinic.
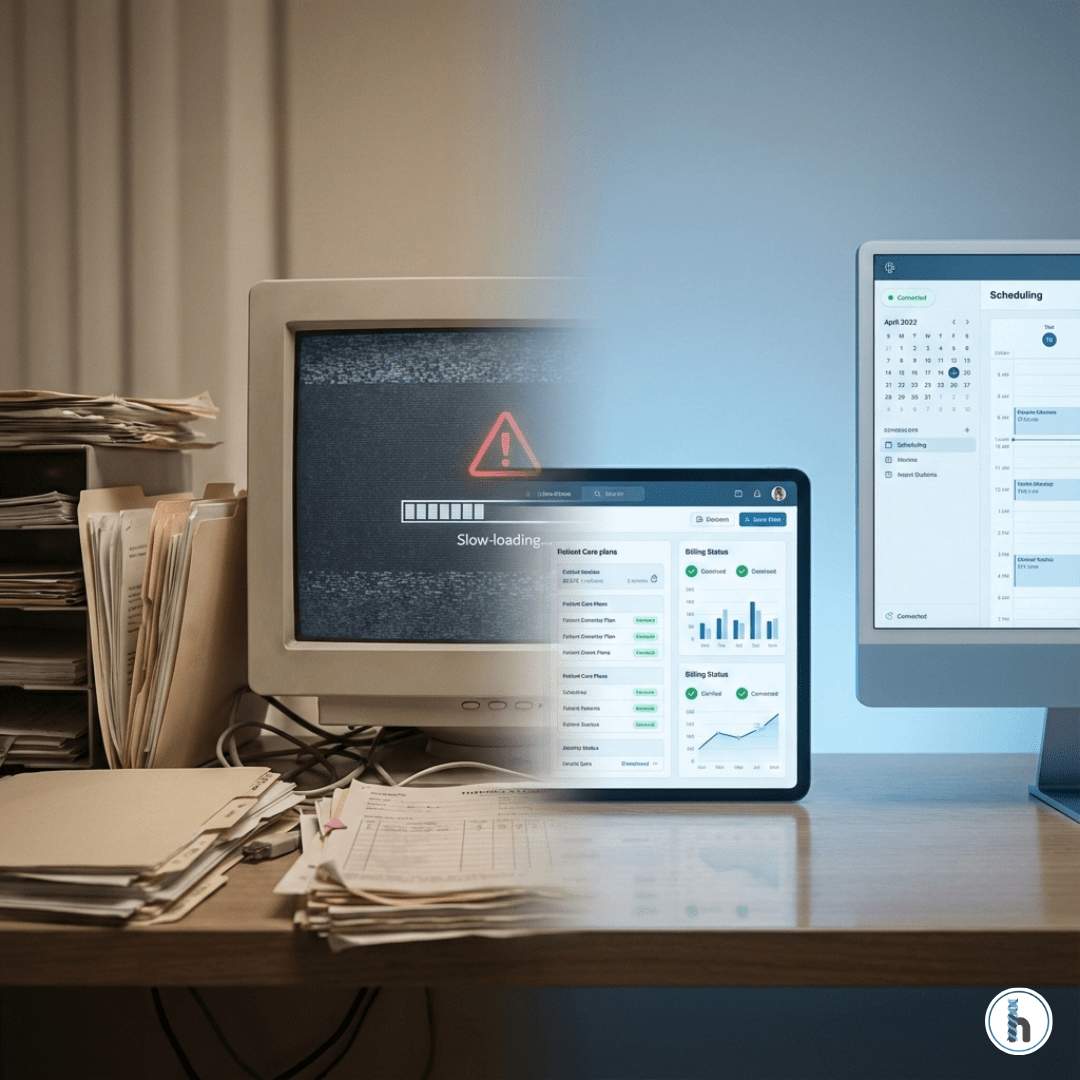
Scheduling and Patient Flow Built for Real Therapy Clinics
HelloNote’s scheduling features are not isolated tools. They work together as a connected system designed around therapy workflows.
From online scheduling and automated reminders to internal alerts and patient status tracking, HelloNote helps clinics:
- Reduce administrative burden
- Improve patient communication
- Protect clinician and staff time
- Support consistent, high-quality care
If your clinic needs scheduling that works with your workflow—not against it—HelloNote is built for therapy practices.
Frequently Asked Questions About Therapy Scheduling Software
Therapy scheduling software helps clinics manage appointments, provider availability, patient communication, and workflow coordination in one system designed specifically for rehab therapy practices.
Automated appointment confirmations and reminders via email and SMS keep patients informed and reduce missed visits caused by forgetfulness or confusion.
Yes. HelloNote allows clinics to offer online scheduling through a secure Patient Portal link on their website.
Yes. Clinics can block time for lunches, meetings, vacations, and administrative tasks directly on the calendar.
Real-time patient status tracking improves coordination between front desk and clinical teams, reduces delays, and helps clinics prioritize next steps like authorizations or discharges.