Medicare Telehealth Extension 2025: Critical Updates for Therapists
Stay updated on the Medicare telehealth extension for 2025 and its impact on therapy practices. Learn about policy updates, supervision changes, and how therapists can continue providing remote care under the Appropriations and Extensions Act, 2025.
The Senate recently passed the Continuing Appropriations and Extensions Act, 2025, which proposes to extend telehealth services for physical therapists, occupational therapists, and speech-language pathologists through September 30, 2025. However, this bill has not yet been enacted into law and still requires approval from the Senate and the President’s signature before taking effect. Until then, the current officially enacted extension remains through March 31, 2025, as previously established under the American Relief Act, 2025.
This extension, if approved, would ensure that therapy providers can continue offering remote services to Medicare beneficiaries, allowing for greater access to care, particularly in rural and underserved areas.
However, this legislation does not include changes to the Medicare Physician Fee Schedule conversion factor, meaning that reimbursement rates remain flat despite rising costs. Therapy professionals must carefully navigate these financial challenges while leveraging new opportunities created by the policy updates.
Key Policy Updates Impacting Therapy Practices in 2025
Extension of Telehealth Services
One of the most significant provisions in the Continuing Appropriations and Extensions Act, 2025, is the temporary extension of telehealth services for therapy providers. Physical therapists, occupational therapists, and speech-language pathologists will be able to continue delivering virtual care to Medicare beneficiaries until September 31, 2025. This is particularly beneficial for reaching patients in rural or underserved areas and for those with mobility challenges.
General Supervision for Therapy Assistants
A major regulatory change in the 2025 final rule allows physical therapists in private practice and occupational therapists in private practice to use general supervision for physical therapist assistants and occupational therapy assistants for all applicable outpatient therapy services. This provides greater flexibility in managing therapy assistants, streamlining practice operations, and enhancing patient care coordination.
Certification of Therapy Plans of Care
CMS has introduced an important exception to the physician/nonphysician practitioner signature requirement for initial therapy plan certifications. If a signed order or referral from a physician/NPP is on file, and the treatment plan is transmitted to the physician/NPP within 30 days of the initial evaluation, the initial certification will be considered valid. This change simplifies administrative requirements for therapy clinics while maintaining physician oversight. However, this exception does not apply to recertifications.
Expansion of Telehealth Services for Caregiver Training
CMS has expanded telehealth coverage to include caregiver training services, recognizing the essential role caregivers play in patient care. New Medicare-approved codes allow therapists to provide training in direct care and behavior management through telehealth. The key additions to the Medicare Telehealth List include:
-
- G0541-G0543: Direct care training services, such as wound care, infection control, diet preparation, and medication administration.
-
- G0539-G0540: Behavior management and modification training for caregivers.
This expansion allows therapy providers to educate caregivers remotely, improving patient outcomes while increasing revenue opportunities for clinics offering these services.
For a more in-depth look at how to navigate caregiver training codes and maximize billing success, visit HelloNote’s guide on updated caregiver training codes for 2025.
Lack of Adjustments to the Medicare Physician Fee Schedule
Despite these advancements, therapy providers will not see an increase in Medicare reimbursement rates in 2025. The MPFS conversion factor will decrease by approximately 2.83 percent, reflecting continued downward pressure on provider payments. This presents financial challenges for therapy clinics already managing increased operational costs. Practices must focus on efficiency, optimized billing processes, and strategic use of telehealth to maintain profitability.
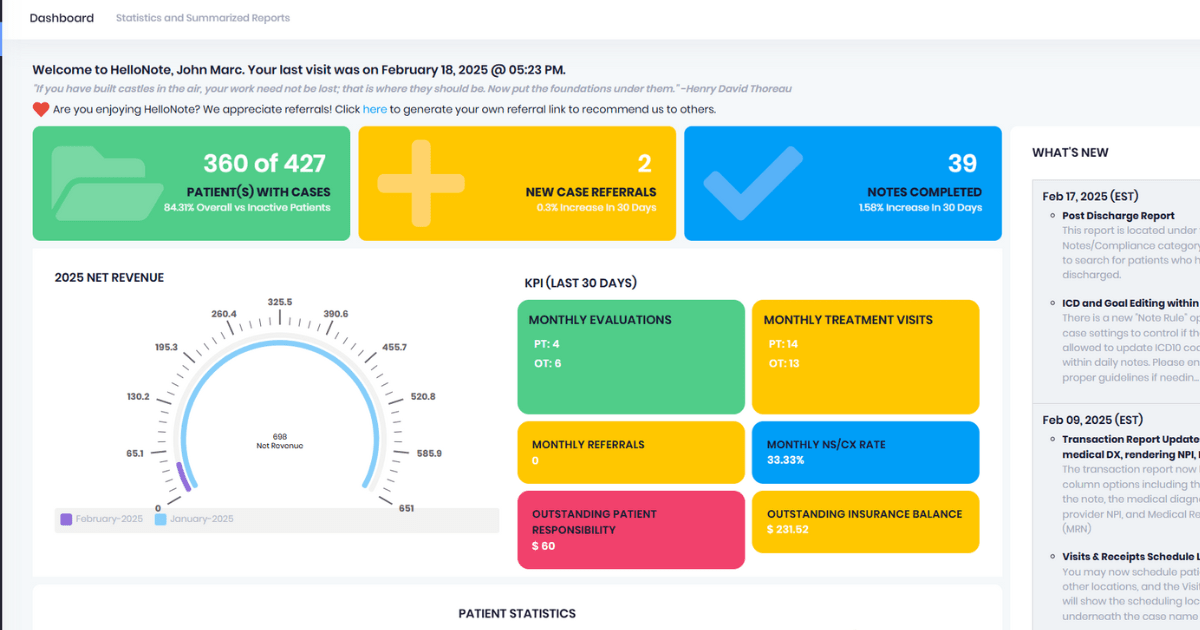
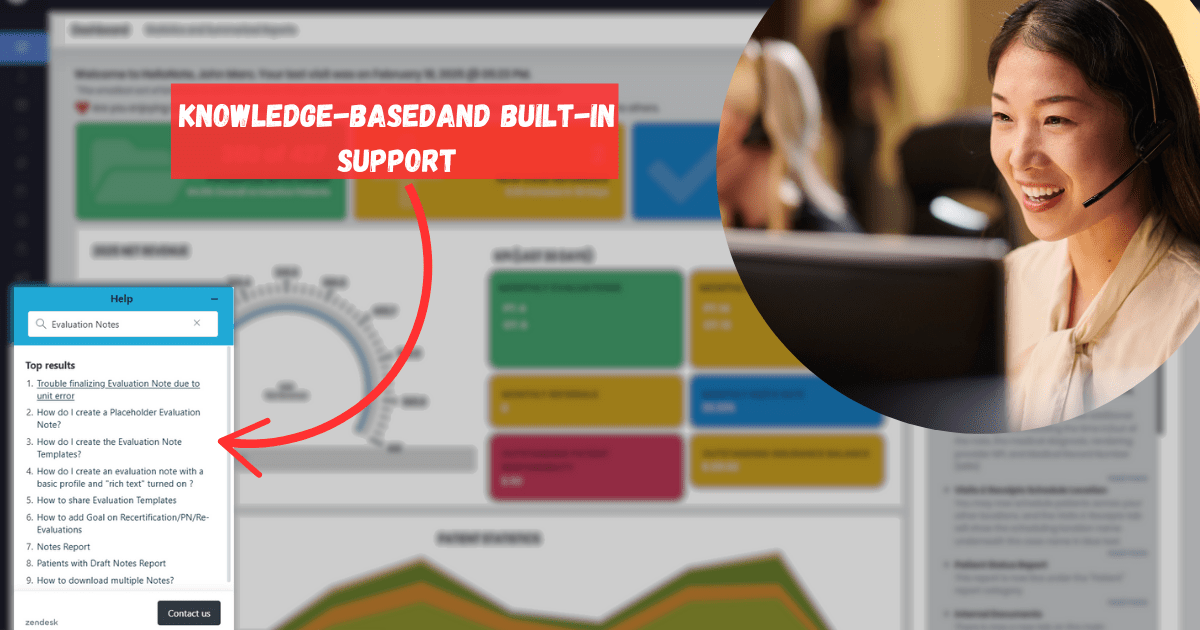
How HelloNote Supports Therapy Practices in 2025
With Medicare reimbursement rates remaining stagnant and operational costs increasing, therapy practices need a system that streamlines workflows and ensures financial stability. HelloNote offers a comprehensive electronic medical record (EMR) solution designed to optimize billing, documentation, and telehealth services while keeping practices compliant with evolving regulations.
Optimized Billing and Faster Reimbursements
HelloNote helps therapists manage claims efficiently with:
-
- Automated claims submission to minimize denials and delays.
-
- Integrated insurance verification tools to prevent errors and ensure proper billing.
-
- Faster reimbursement processing, improving cash flow for therapy clinics.
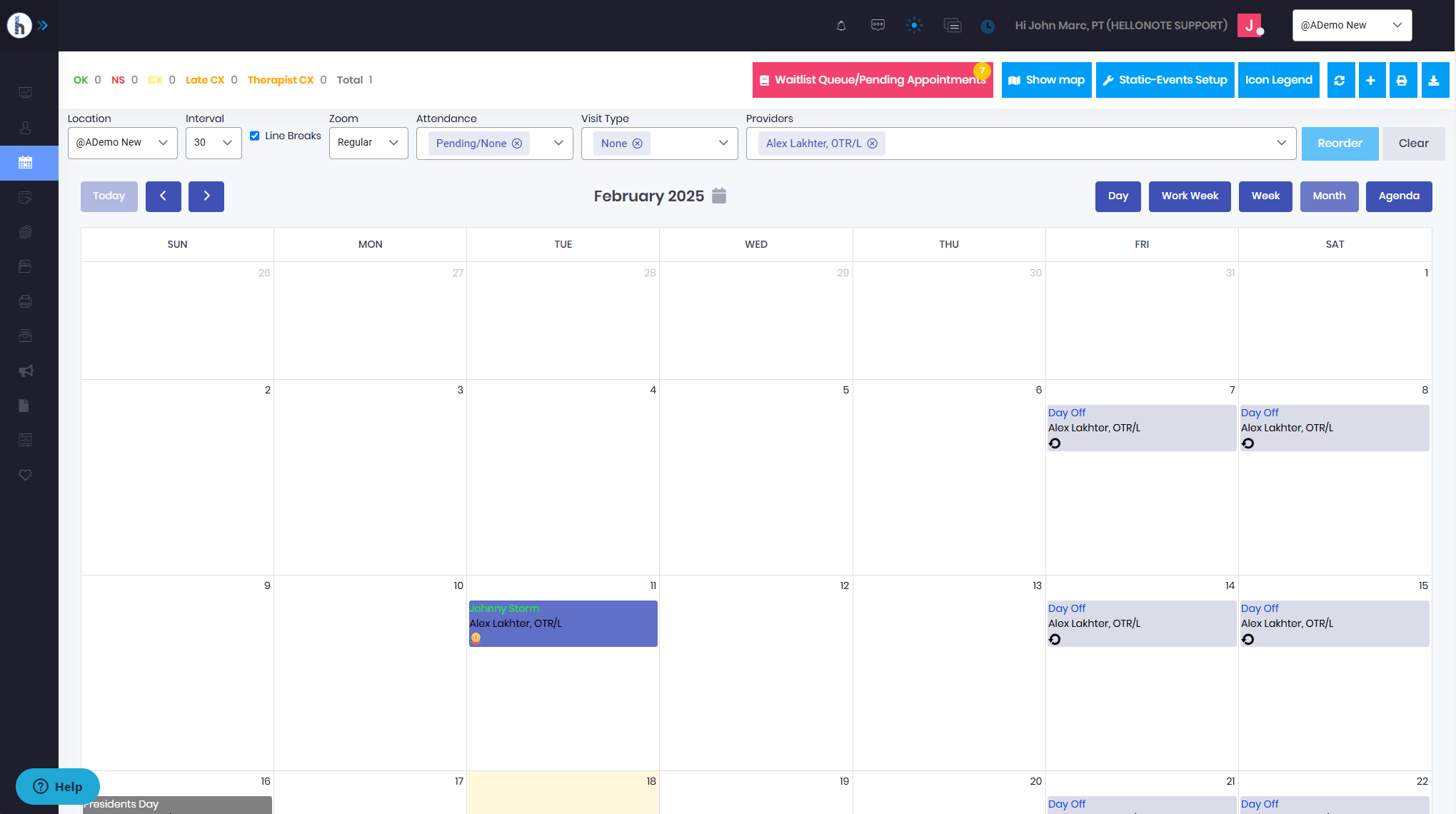
Seamless Telehealth Capabilities
With telehealth extended through September 2025, therapy providers must ensure they have the right tools for virtual care. HelloNote’s built-in telehealth features enable therapists to:
-
- Conduct HIPAA-compliant virtual sessions.
-
- Seamlessly document telehealth visits for Medicare compliance.
-
- Expand patient access to therapy services beyond geographic limitations.
Support for Therapy Assistants
With the shift to general supervision for PTAs and OTAs, therapy clinics can structure their services more efficiently. HelloNote provides intuitive scheduling and workflow management tools to support this transition while maintaining compliance with supervision requirements.
Simplified Certification and Documentation
With the new exception for initial therapy plan certifications, practices must ensure they have an efficient documentation system. HelloNote provides:
-
- Secure storage and transmission of treatment plans to meet Medicare requirements.
-
- Tracking tools to document physician orders and referrals.
-
- Pre-built compliance templates that streamline administrative tasks.
Preparing for the Future of Therapy Practice Management
The Continuing Appropriations and Extensions Act, 2025, brings both opportunities and challenges for therapy providers. The telehealth extension and expanded caregiver training services allow therapists to reach more patients and provide additional services. However, the lack of reimbursement increases means practices must focus on efficiency and cost management to stay financially sustainable.
HelloNote is designed to help therapy practices navigate these changes effectively. By integrating smart billing, telehealth tools, and compliance-friendly documentation, therapy providers can focus on delivering quality care while optimizing financial performance.
Therapists looking to adapt to the latest Medicare updates can explore how HelloNote supports compliance, efficiency, and financial success.