Medicare Billing Guide for PT & OT: 2026 Compliance & Documentation Updates
Table of Contents
Introduction
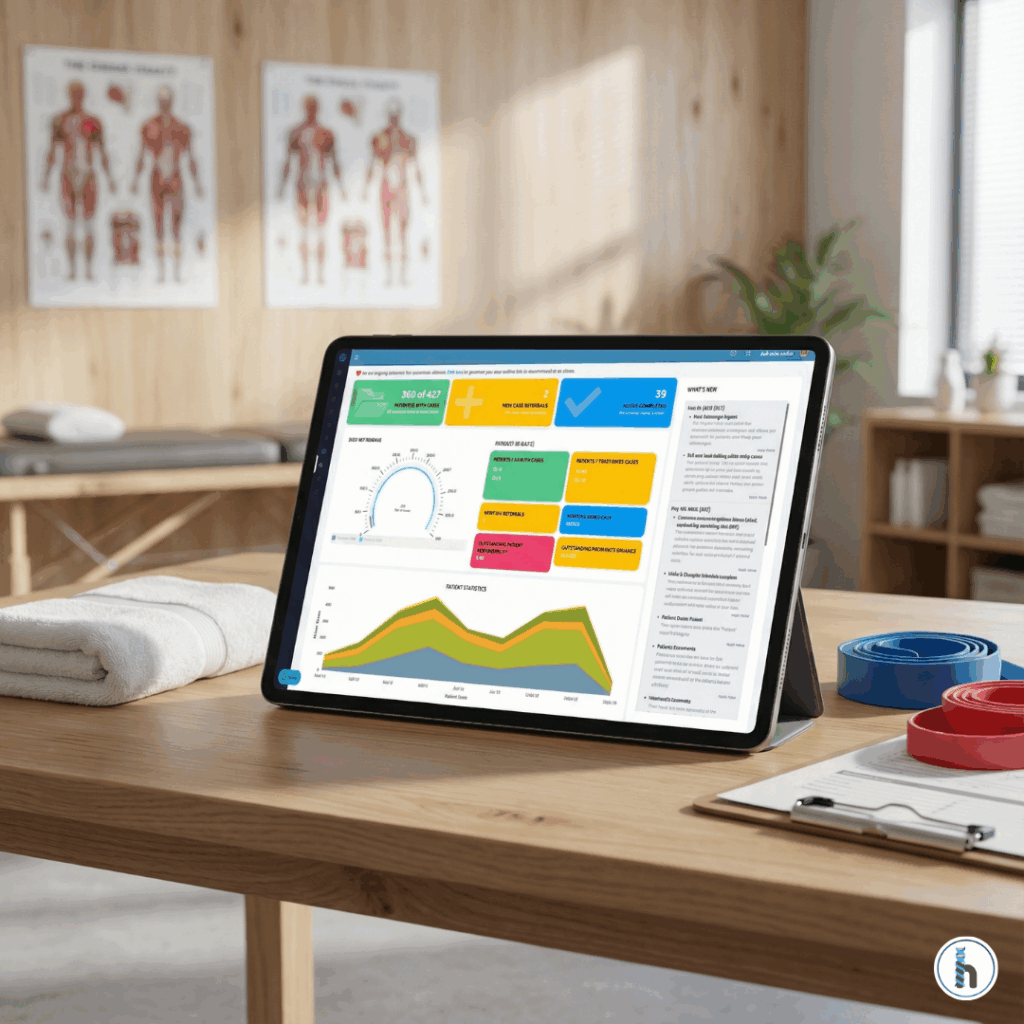
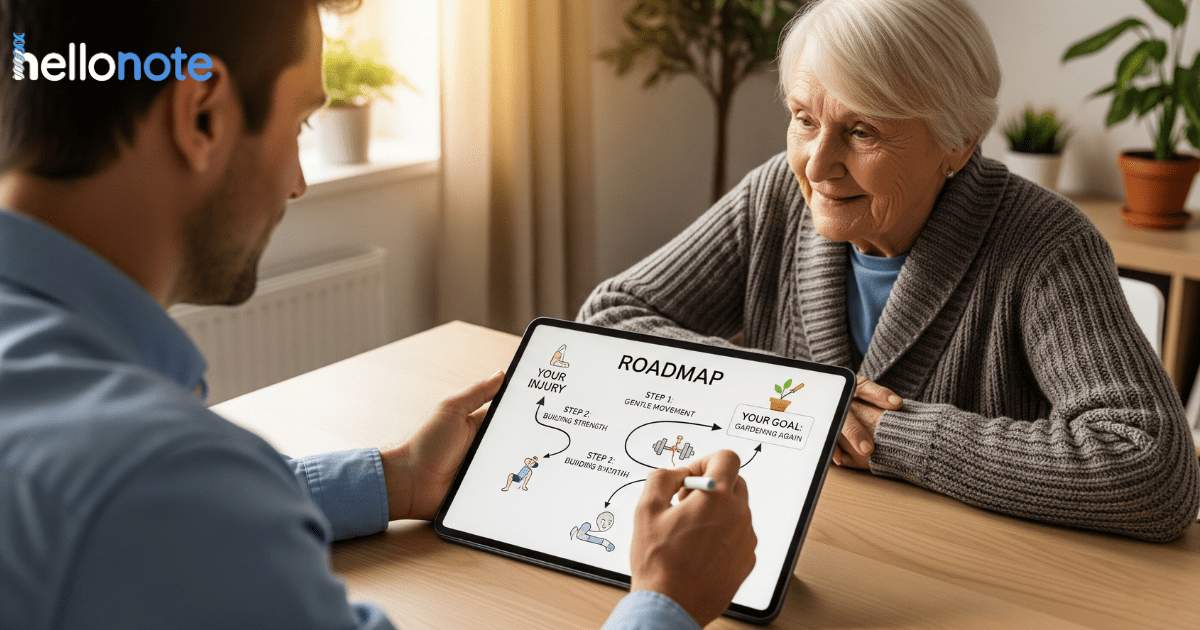
Navigating Medicare’s intricate billing and documentation requirements for physical therapy (PT) and occupational therapy (OT) services can often feel like a complex maze for even the most seasoned therapy practices. Staying current with updates and adhering to best practices is crucial not only for compliance but also for ensuring accurate billing and timely reimbursement. This guide, drawing on insights from recent Medicare updates and expertise from the Billing team, aims to be your go-to Medicare Billing Guide for Therapy Practices. We will cover essential topics such as medical necessity, comprehensive Medicare Documentation Requirements PT OT, therapy caps, coding guidelines, and key Therapy Medicare Compliance 2026 updates to help your practice thrive. For practices utilizing an EMR, understanding how your system, like HelloNote EMR Medicare Billing features, can support these processes is invaluable.
Key Takeaways for 2026
- 2026 KX Threshold: The threshold has increased to $2,480 for PT/SLP combined and $2,480 for OT.
- General Supervision: Outpatient private practices can now use general supervision for PTAs and OTAs, providing significant staffing flexibility.
- RTM Flexibility: New codes 98985 and 98984 now allow billing for monitoring periods of only 2–15 days, down from the previous 16-day requirement.
- Physician Fee Schedule (PFS): While the conversion factor saw a slight increase, net reimbursement for many therapy codes remains largely stagnant due to RVU adjustments.

Medical Necessity & The Critical Role of the Plan of Care
What is Medical Necessity in Therapy?
At its core, Medicare defines medical necessity as services that are reasonable and necessary for the diagnosis or treatment of an illness or injury, or to improve the functioning of a malformed body member. For therapy services, this means the treatment must be of a level of complexity and sophistication that requires the skills of a licensed therapist. Your documentation must clearly show that the patient’s condition requires skilled intervention and that they are making—or have the potential to make—functional progress.
Essential Plan of Care (POC) Requirements
A valid, comprehensive Plan of Care is the bedrock of Medicare billing for therapy services. According to Medicare guidelines, a POC must be established before treatment begins and must include:
- Diagnoses: Specific to the condition being treated.
- Long-term Treatment Goals: Must be measurable and functional.
- Type, Amount, Duration, and Frequency: Clearly defined (e.g., Therapeutic Exercise 2x/week for 8 weeks).
- Signature & Date: The therapist who established the plan must sign and date it immediately.
Navigating Certifications, Recertifications & Authorizations
Initial Certification Nuances
Medicare mandates that the initial Plan of Care be certified by a physician or NPP within 30 calendar days of the therapy evaluation. While a written order or referral is helpful, it does not replace the need for a signed POC. 2026 Pro-Tip: CMS now allows for an “exception to signature” if you have documented evidence that the POC was sent to the MD/NPP within 30 days and you are awaiting the return, provided a referral is already on file.
Recertification Timing
The POC needs to be recertified at least every 90 calendar days from the date of the initial certification. However, if there is a significant change in the patient’s condition or the treatment goals, a new certification should be obtained immediately to remain compliant.
Mastering Medicare Billing & Coding Guidelines
Timed vs. Untimed CPT Codes
Correctly differentiating and documenting timed versus untimed codes is fundamental.
- Untimed Codes (Service-Based): These include evaluations (97161-97163) and certain modalities like unattended E-stim. You bill one unit regardless of how long the service takes.
- Timed Codes (Time-Based): These include therapeutic exercise (97110) and manual therapy (97140). These follow the 8-Minute Rule.
The Medicare Therapy Cap & Proper KX Modifier Use
Understanding the 2026 Thresholds
Technically, the “Therapy Cap” was repealed, but it was replaced by the KX Modifier Threshold. For 2026, the threshold is $2,480 for PT and SLP combined, and $2,480 for OT.
- The KX Modifier: By appending this modifier, you are attesting that the services are medically necessary and justified by your documentation.
- Medical Review Threshold: Once a patient exceeds $3,000 in spend, they enter the “Targeted Medical Review” zone. While not an automatic audit, these claims are more likely to be scrutinized by Medicare Administrative Contractors (MACs).
2026 Update: Remote Therapeutic Monitoring (RTM)
Medicare has expanded digital health flexibilities for 2026 to help clinics capture more revenue from home-based care.
- New Code 98985: Device supply for musculoskeletal monitoring for 2–15 days in a 30-day period. (Previously, only 16+ days were billable).
- New Code 98979: RTM treatment management for the first 10 minutes of therapist time in a month.
- Documentation Requirement: You must document the specific device used and the therapist’s clinical interpretation of the data transmitted.
Frequently Asked Question
The threshold is $2,480 for PT/SLP combined and $2,480 for OT.
Yes. CMS has permanently authorized General Supervision in outpatient private practices. The supervising therapist must be available but is not required to be on-site.
Medicare requires a progress report at least once every 10 treatment days. This report must be completed by a licensed therapist, not an assistant.
For the original RTM codes, yes. However, new 2026 codes (98985) allow for billing musculoskeletal monitoring with as little as 2–15 days of data.
A re-evaluation is only billable when there is a significant change in the patient’s functional status or if a new clinical condition arises that requires a revised Plan of Care.