Discover the best alternative EMR for your therapy practice with HelloNote. Designed specifically for physical, occupational, and speech therapists, HelloNote simplifies scheduling, documentation, and billing all in one platform. Say goodbye to complicated, generic systems and switch to a streamlined, user-friendly solution that improves efficiency and enhances patient care. Optimize your practice today with HelloNote – the EMR built with your clinic’s needs in mind.
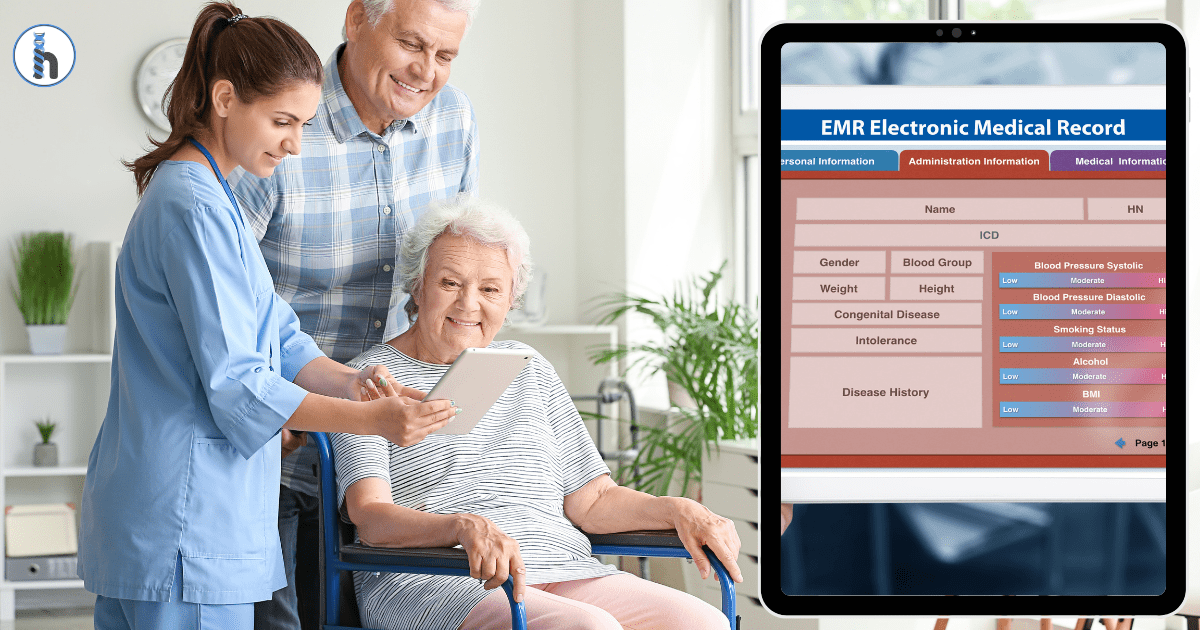
Switching your clinic’s Electronic Medical Record (EMR) system is a big decision that comes with its challenges. While new features and improved workflow are enticing, the process can be complicated with disruptions, data transfer delays, and system outages.
These issues can add up, especially when dealing with contract obligations, integration problems, and the learning curve for staff. Without careful planning, switching EMRs can impact your clinic’s operations, slow down your workflow, and strain resources.
Choosing the wrong EMR could lead to long-term consequences, affecting your clinic’s success. That’s why it’s essential to select a platform that seamlessly integrates into your workflow and meets the specific needs of your therapy practice.
This guide is designed to help you make an informed decision when choosing an EMR, so you don’t end up locked into a restrictive contract that doesn’t meet your needs.
wpDataTable with provided ID not found!
Why Choose HelloNote over WebPT, SimplePractice, Prompt, JaneApp, System4PT, PTEverywhere, Spry, Heno, Raintree Inc, Theraplatfor.
Designed for Therapists: Specialization Matters
HelloNote is for Therapy Professionals
We understand the unique challenges that physical therapists, occupational therapists, and speech-language pathologists face because we’ve been in your shoes. Our platform isn’t a generic EMR trying to fit all healthcare providers — it’s designed specifically for therapy professionals, ensuring that every feature supports the way you work.
This isn’t just a marketing claim; it’s embedded in everything we do. From customized documentation templates to streamlined workflow management, our system is built to enhance efficiency, simplify compliance, and improve patient outcomes. We know what therapists need, and we’ve designed HelloNote to deliver exactly that.
Client Testimonials: Real Therapists, Real Benefits
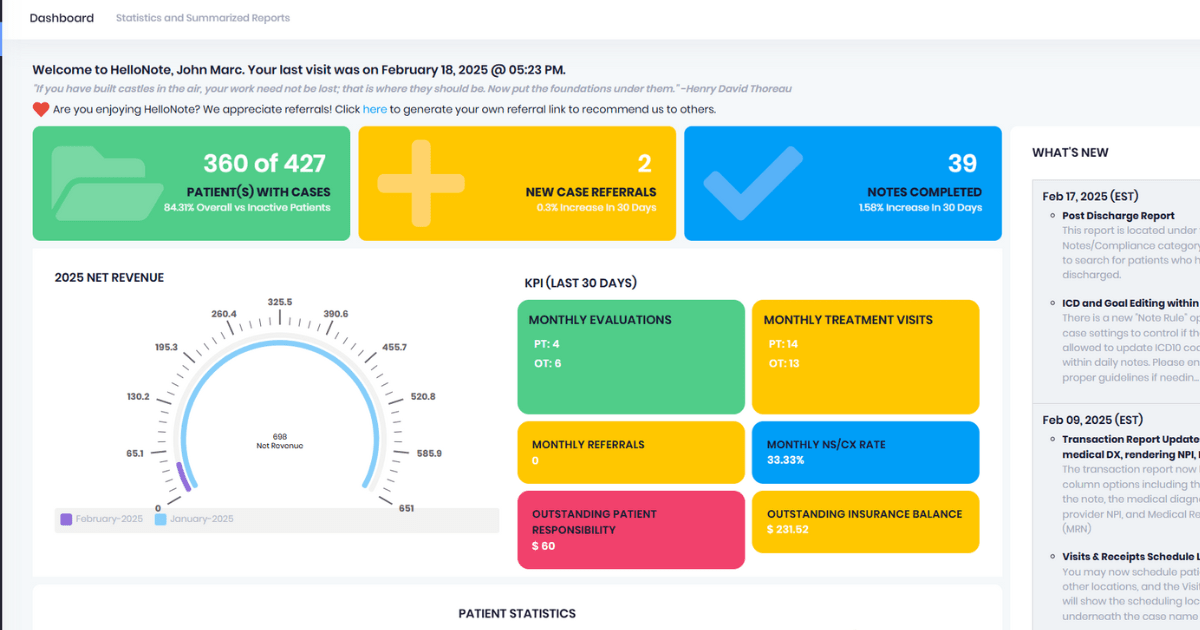
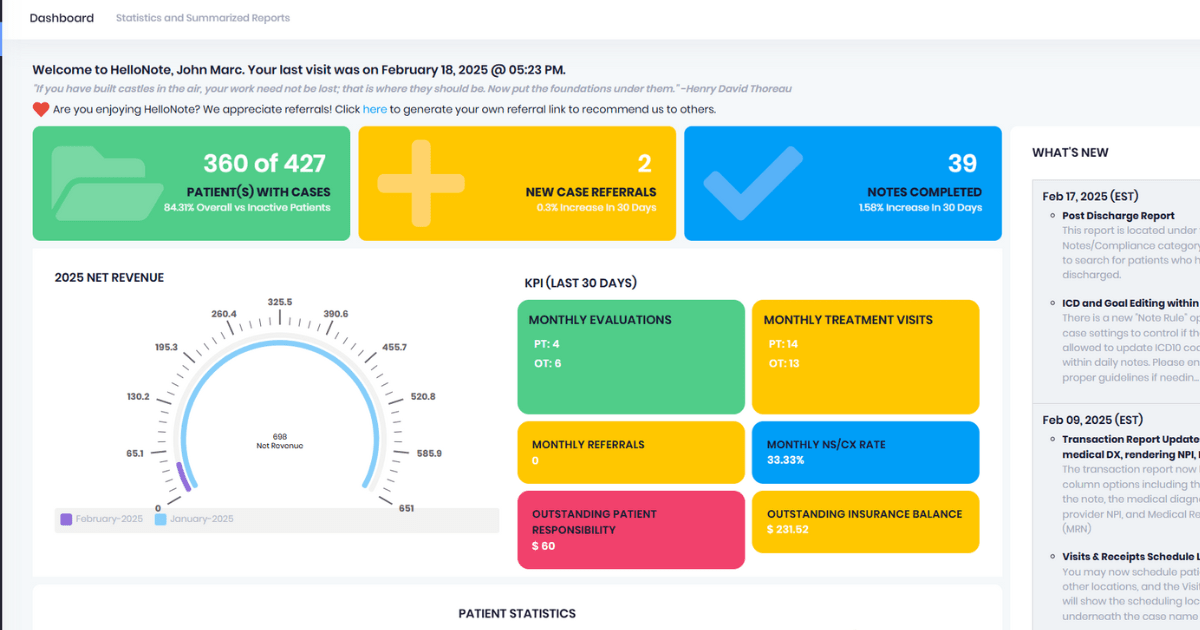
One of the standout features of HelloNote is its user-friendly dashboard, which allows therapy professionals to access key information quickly and efficiently. A client recently shared their experience:
“I love the dashboard feature because it summarizes everything I need to know. There’s probably even more that I haven’t explored, but the basics are right there. For example, I can easily track when we need to recertify patients, especially since we see many patients with neurologic conditions for longer durations. The dashboard helps me stay on top of when plans of care need updates and whether the doctor has signed off. It also shows me if we’ve received necessary documents, making everything very streamlined and easy to manage. The system is easy to navigate, and the team has been amazing with support. Since switching to HelloNote, the billing process has been a lot easier. It’s been light years easier for me, and I now handle billing for our whole team. It’s fast, efficient, and truly made my life easier!” DR. Chloe Diordano PT, DPT Founder and Owner of Neuro Nation Physical Therapy and Wellness.
This testimonial highlights how HelloNote’s intuitive dashboard and billing features can simplify daily operations for therapy practices, particularly those managing long-term care or dealing with complex documentation needs. The ease of use and quick navigation save valuable time, allowing therapists to focus on patient care instead of administrative tasks.
Integration and Streamlining
At HelloNote, we know that therapists don’t have time to juggle multiple systems for scheduling, documentation, and billing. That’s why we built an all-in-one EMR that seamlessly integrates these essential functions into a single, streamlined platform. By eliminating the need for third-party add-ons, we help reduce inefficiencies, minimize errors, and keep your workflow as smooth as possible. Our goal is to provide a solution that lets you focus on patient care, not software workarounds.
Billing Transparency & Pricing Comparison
How HelloNote Simplifies Billing for Therapists
We know that billing shouldn’t be a guessing game. As therapists ourselves, we’ve seen how complicated and frustrating insurance claims and payments can be, especially for small to mid-sized practices. That’s why we built a billing system that prioritizes transparency, affordability, and ease of use.
HelloNote’s pricing structure is designed to keep things straightforward, without hidden fees or surprise charges. We don’t believe in adding extraneous features that would increase your monthly bill without providing meaningful value to your practice. Our focus is on providing you with the tools and functions that directly support your day-to-day operations. By avoiding unnecessary complexities, we ensure that you only pay for the features that truly benefit your practice.
With one-click claims generation, seamless insurance processing, and a pricing model that fits the needs of therapy clinics, we make it easy to manage your finances efficiently. No more paying for features you don’t need, just the solutions that work for you.
“ 100%. I would say again, I don’t know how those scaling works. However, if it works for one person, it’s going to work for everybody. Right? It’s simple. I’ve used every single, uh, documentation system known to man working in hospitals with Epic, working in practices with everything from, uh, prompt to, you know, WebPT, but again.
Everything has different features, but hello note is by far the most simple and easy to use and direct. And that’s what I want as a practitioner. And again, from a price point, you guys were the only people that would let me come on as a sole practitioner. So I’m super grateful for that. And again, regardless, like the cost is honestly very, very, very affordable.
And it essentially, I mean, if, again, it makes me money essentially, because I’m able to, yeah. Have more clients, build more with confidence, get those things. You guys have great support. So yeah, I’m super grateful. That’s why I chose to, you know, kind of do the interview. I was like, you know what, they’ve been really good to me.
And even at, I was at PPS and I saw you guys at a booth and then I talked to, I can’t remember her name, but she was a really sweet lady from New York. And I was like, Oh yeah, you guys are great. I love you guys so much. And I, you know, and I said, Hey, you know, I paid a year in full. Can you guys give me like, you guys want, she was like, yeah, I’ll take care of you.
Don’t worry. And she like emailed me, you know, the next week. So just having that like relationship of just trusting the real people it’s, it’s fantastic. So I appreciate your all’s work. And like I said, that’s part of the reason why I wanted to come on here today. Cause I’m a huge advocate for hello note and I grateful for the kind of opportunity it’s given me, because like I said, I’m very happy and I don’t need to change a thing right now.
So, and even if I expanded, I would know I’d be able to do that confidently with you guys.”
Daniel C Brown, DPT, COMT, OCS owner of DCB Physical Therapy.
Telehealth & Patient Engagement
How HelloNote Elevates Telehealth and Patient Engagement
Virtual therapy isn’t just a convenience but a necessity. Whether you’re working with remote patients, managing home health visits, or offering hybrid care, having a seamless, HIPAA-compliant telehealth solution is essential. That’s why we’ve built integrated telehealth directly into our platform, along with a secure patient portal that enhances engagement and accessibility.
Scheduling & Documentation: Reducing Admin Burden
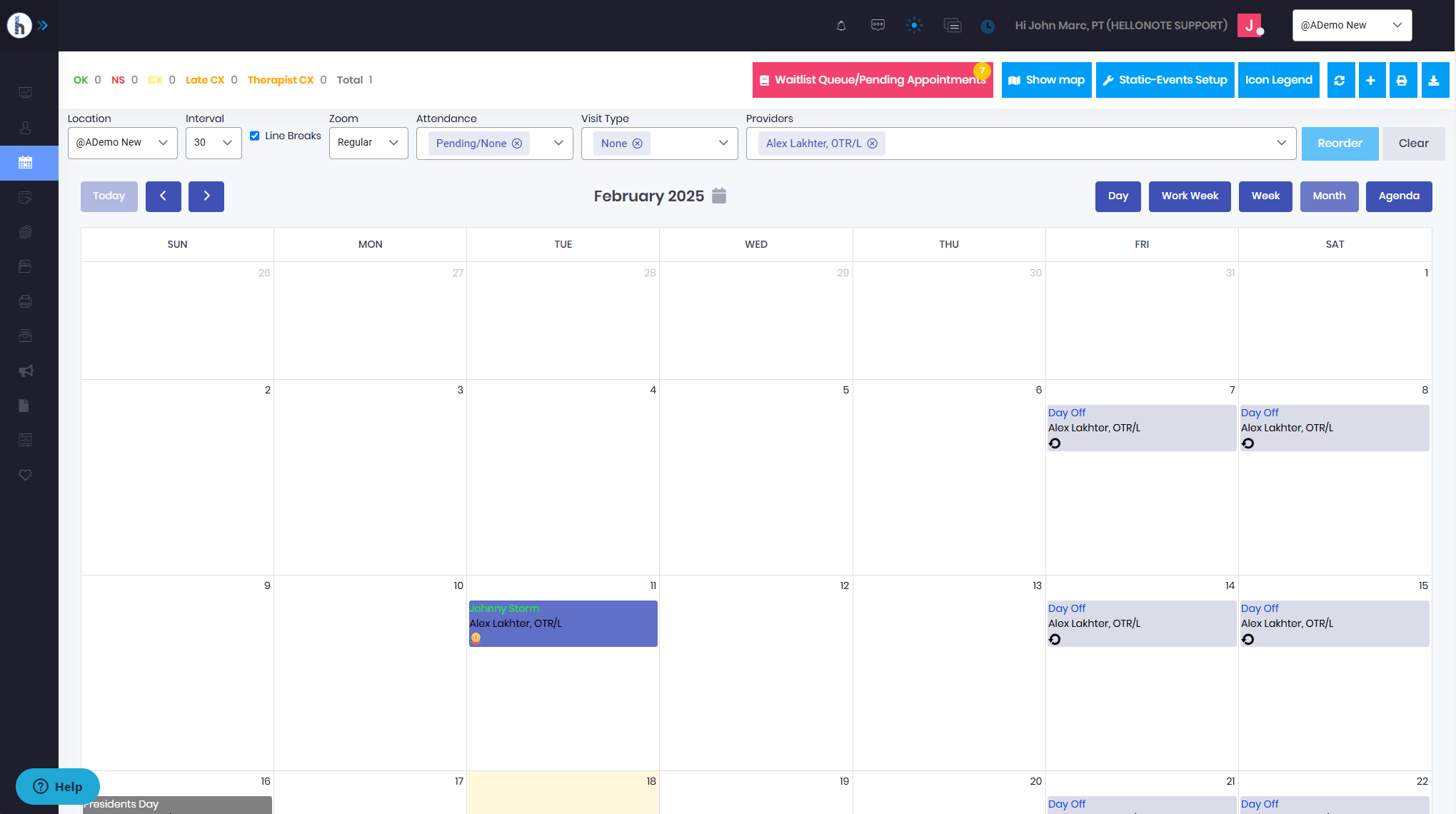
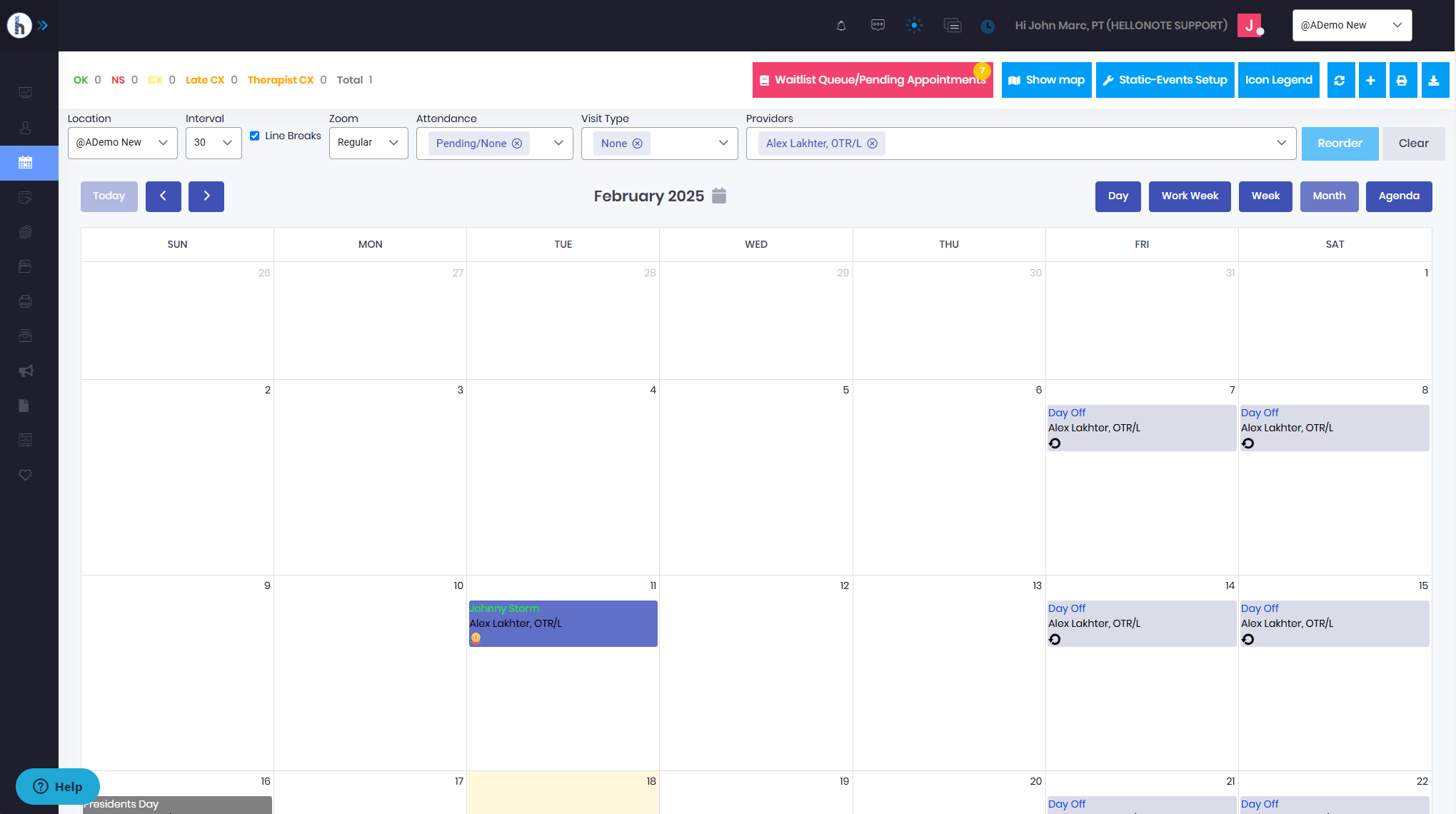
How HelloNote Simplifies Scheduling and Documentation for Therapists
At HelloNote, we know that efficient scheduling and documentation are essential for a smooth workflow. As therapists ourselves, we’ve seen how frustrating it can be when scheduling tools don’t align with real-world therapy needs or when documentation feels like a time-consuming chore instead of a helpful tool.
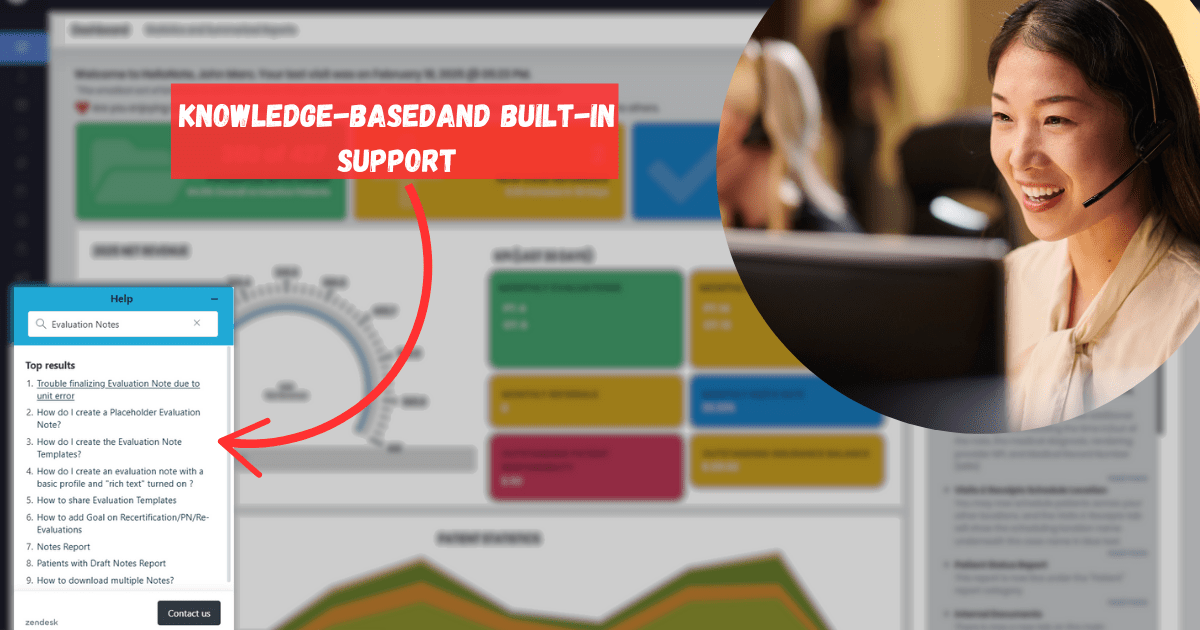
Customer Support & Community Feedback
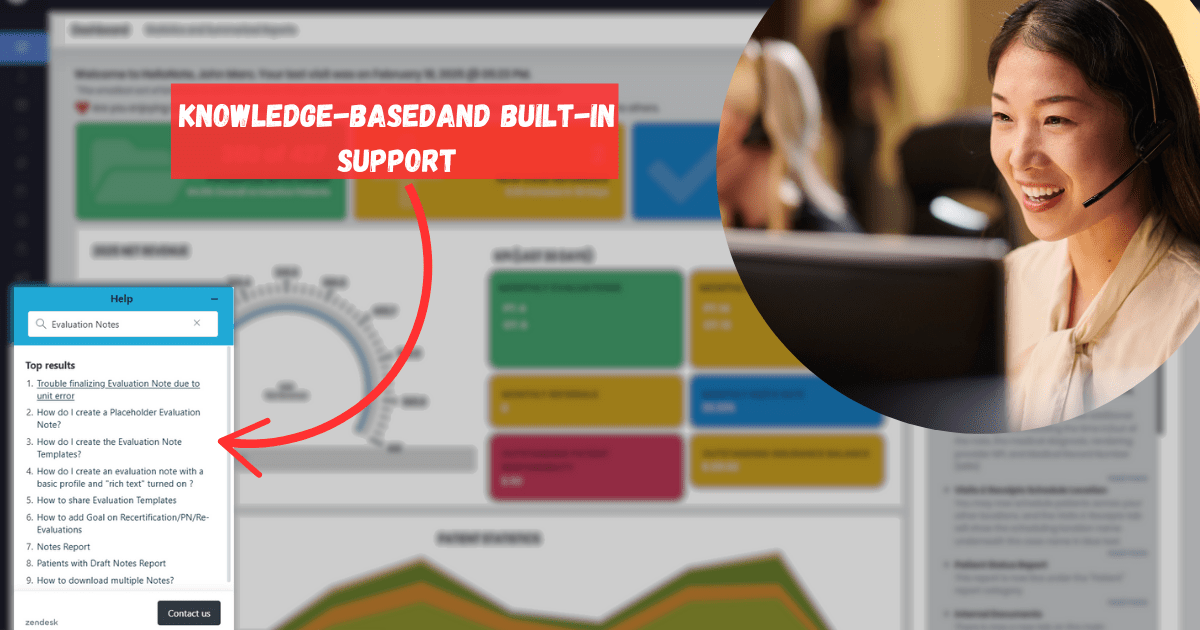
HelloNote: Responsive Support & Continuous Updates
We know that having a reliable support team isn’t just a nice-to-have but essential. Therapists don’t have time to wait on hold for hours or deal with unanswered support tickets when they need immediate assistance. That’s why we’ve built a responsive, knowledgeable support team that is readily available to help whenever you need it.
Another client shared their experience with HelloNote’s support and commitment to improvement:
“You guys have been pivotal to us. I’ve really enjoyed the communication and collaboration on building reports that we need and changing things within the EMR. For example, the new map feature where we can see where our clinicians are seeing patients is going to be a game-changer for us. You’ve been incredibly open to feedback, and we can’t thank you enough!” Dr. Derek Smith – PT, DPT, GCS of Roaming Rehab
This feedback illustrates HelloNote’s commitment to continuous improvement and the platform’s flexibility to adapt to the unique needs of each therapy practice.
Addressing Security and Compliance
HIPAA Compliance and Data Security in HelloNote
We understand how critical patient data security is, and we take it seriously. HelloNote is fully HIPAA-compliant, ensuring that your practice and your patients’ sensitive information are protected with the highest security standards.
7 Common Mistakes to Avoid When Choosing an EMR for Your Therapy Practice
- Choosing a Generic EMR Instead of One Tailored for Therapy
Many EMR systems are designed for general healthcare practices and don’t offer the specialized features that therapy clinics require. Always choose an EMR that is built specifically for physical, occupational, and speech therapy practices. Look for features like customizable documentation templates, therapy-specific progress tracking, and the ability to manage long-term treatment plans.
- Neglecting Integration Capabilities
An EMR that doesn’t integrate smoothly with your other software systems can create inefficiencies and lead to errors. Ensure the EMR you choose integrates with scheduling, billing, and patient management systems to streamline operations and improve productivity.
- Overlooking Data Security and HIPAA Compliance
Patient data security is essential. Choose an EMR that guarantees compliance with HIPAA standards, provides encrypted storage, and offers secure data exchange protocols to protect patient confidentiality and ensure compliance with privacy regulations.
- Forgetting About Training and Ongoing Support
No matter how powerful the EMR, it will be ineffective without proper training and reliable customer support. Ensure the system you choose offers comprehensive training materials and accessible, responsive support teams to help you and your staff effectively use the software.
- Opting for an Overly Complex System
Some EMR systems are overly complex, making them difficult to learn and use. Avoid systems that are packed with features your clinic doesn’t need. Select an EMR that strikes the right balance between ease of use and necessary functionality.
- Ignoring the Total Cost of Ownership
The initial cost of the EMR is just one part of the equation. Consider the total cost of ownership, which includes recurring fees for updates, support, and training. Choose a system with clear and transparent pricing to avoid unexpected costs in the future.
- Underestimating the Need for Streamlined Billing, Documentation, and Scheduling
Many therapists struggle with managing patient documentation, scheduling, and billing in separate systems that don’t communicate with each other. This leads to inefficiencies, errors, and extra administrative work. HelloNote offers an integrated solution that combines billing, documentation, and scheduling into one easy-to-use platform, saving time and reducing the likelihood of errors, so you can focus on patient care instead of administrative burdens.
By avoiding these common mistakes, you’ll be better equipped to select an EMR system that fits your clinic’s unique needs, helping you streamline operations, reduce administrative burdens, and ensure long-term success.
Final Verdict: Choosing the Right EMR for Your Therapy Practice
The decision between HelloNote and other platforms hinges on your unique needs and priorities. It isn’t just about features but also about finding a system that fits your workflow without unnecessary complexity or extra costs. With HelloNote, you’ll get a platform that was built by therapists, for therapists, and one that keeps your practice running smoothly while saving you time, money, and energy.
Make the switch to HelloNote today and experience the difference it can make for your therapy practice.