Better Rehab Outcomes Through EMR-Facilitated Care Plans Using Care Plan Software
Table of Contents
Care plans shape every decision therapists make in rehab. They are your roadmap defining goals, guiding interventions, tracking progress, and ensuring payer compliance. But in many clinics, care plans become stagnant documents buried inside the EMR instead of active tools that drive outcomes.
This is where modern care plan software makes the difference.

A strong EMR shouldn’t just store your plan of care. It should activate it bringing goals, progress, and interventions into your daily workflow. That’s exactly how HelloNote is designed: to help therapists build better care plans, document with intention, and support real-time decision-making.
Why the Care Plan Matters in Rehab
Across PT, OT, and SLP settings, the care plan provides the foundation for:
Setting measurable, meaningful goals
Ensuring each session builds toward functional change
Documenting medical necessity for payers
Supporting communication with caregivers and providers
Improving transparency for families, schools, and case managers
But when care plans aren’t supported by effective care plan software, therapists run into predictable obstacles:
Notes become disconnected from goals
Progress isn’t consistently tracked
Reassessments get missed
Documentation becomes reactive instead of strategic
This not only affects workflow it affects patient outcomes.
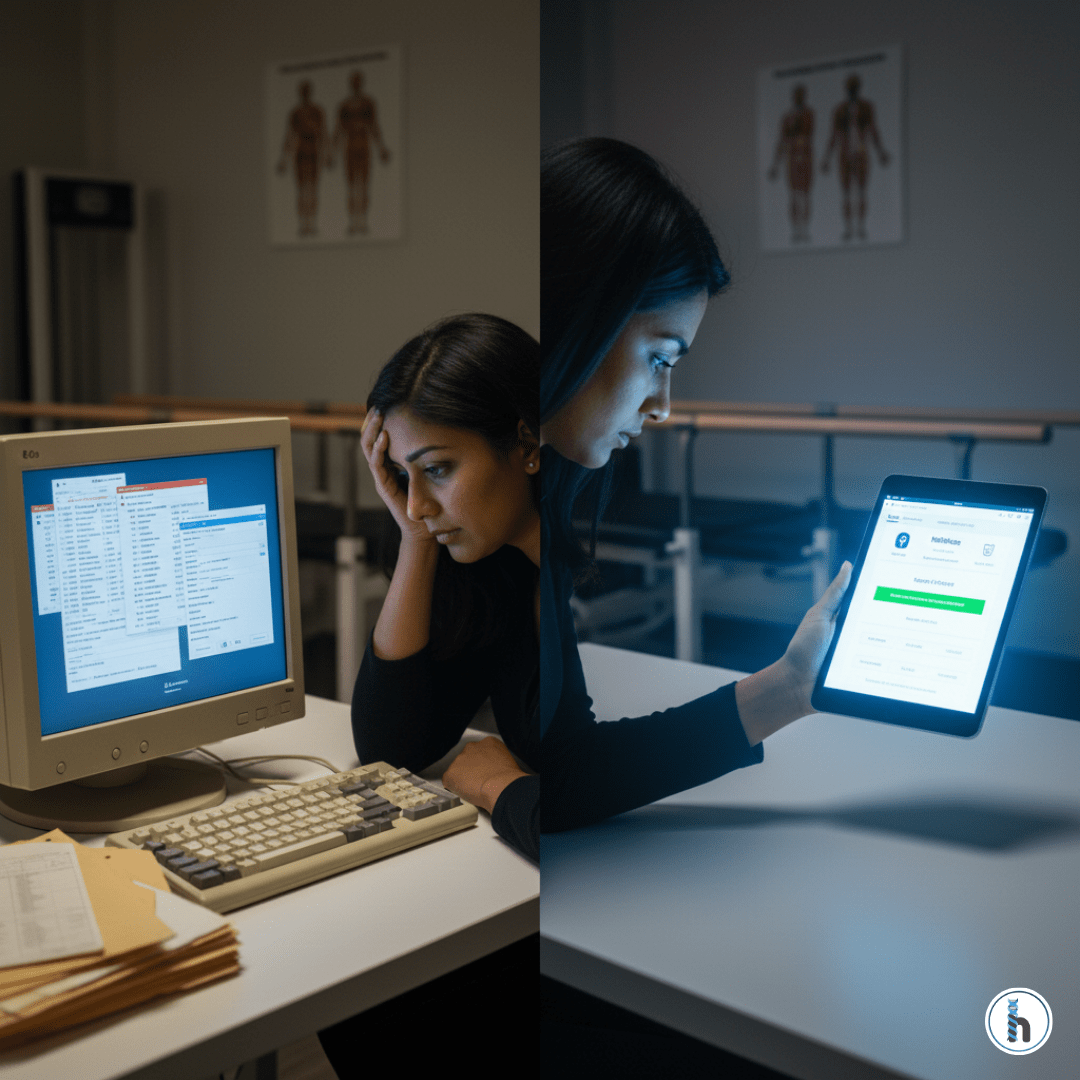
The Problem EMRs That Don’t Support the Care Plan
Many therapists still work in systems that:
❌ Hide the care plan in a disconnected module
❌ Make goal review time-consuming
❌ Don’t offer real-time progress visibility
❌ Require double documentation for billing
Without supportive care plan software, therapists are left juggling spreadsheets, sticky notes, and duplicated entries just to stay organized
How HelloNote Activates the Care Plan (Not Just Stores It)
Modern clinics need care plan software that integrates into workflow does not add friction. HelloNote was built to solve that problem.
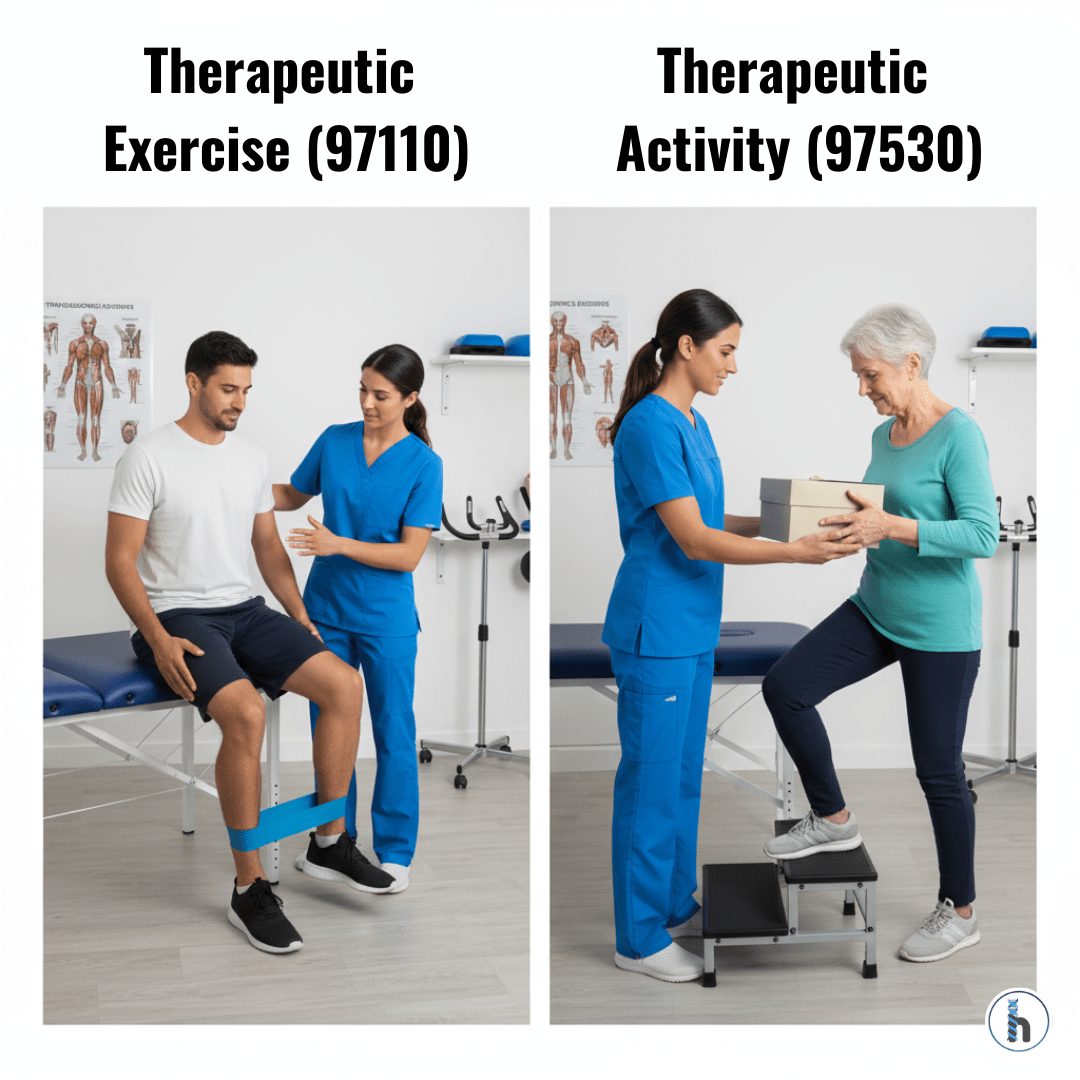
1. Care Plans That Stay Visible and Accessible
In HelloNote, goals never get buried. You can:
Pin the most important goals
View objectives within daily notes
Update progress with one tap
Track CPT alignment alongside goals
The care plan becomes a living tool that shapes each session.
2. Templates Designed for Rehab Disciplines
HelloNote’s templates are made specifically for:
Physical therapists
Occupational therapists
Speech therapists
Including:
Functional goals
GAS scoring
Pediatric and developmental milestones
IEP-aligned structures
This is caring plan software designed by clinicians, not generic developers.
3. Real-Time Progress Tracking for Better Decisions
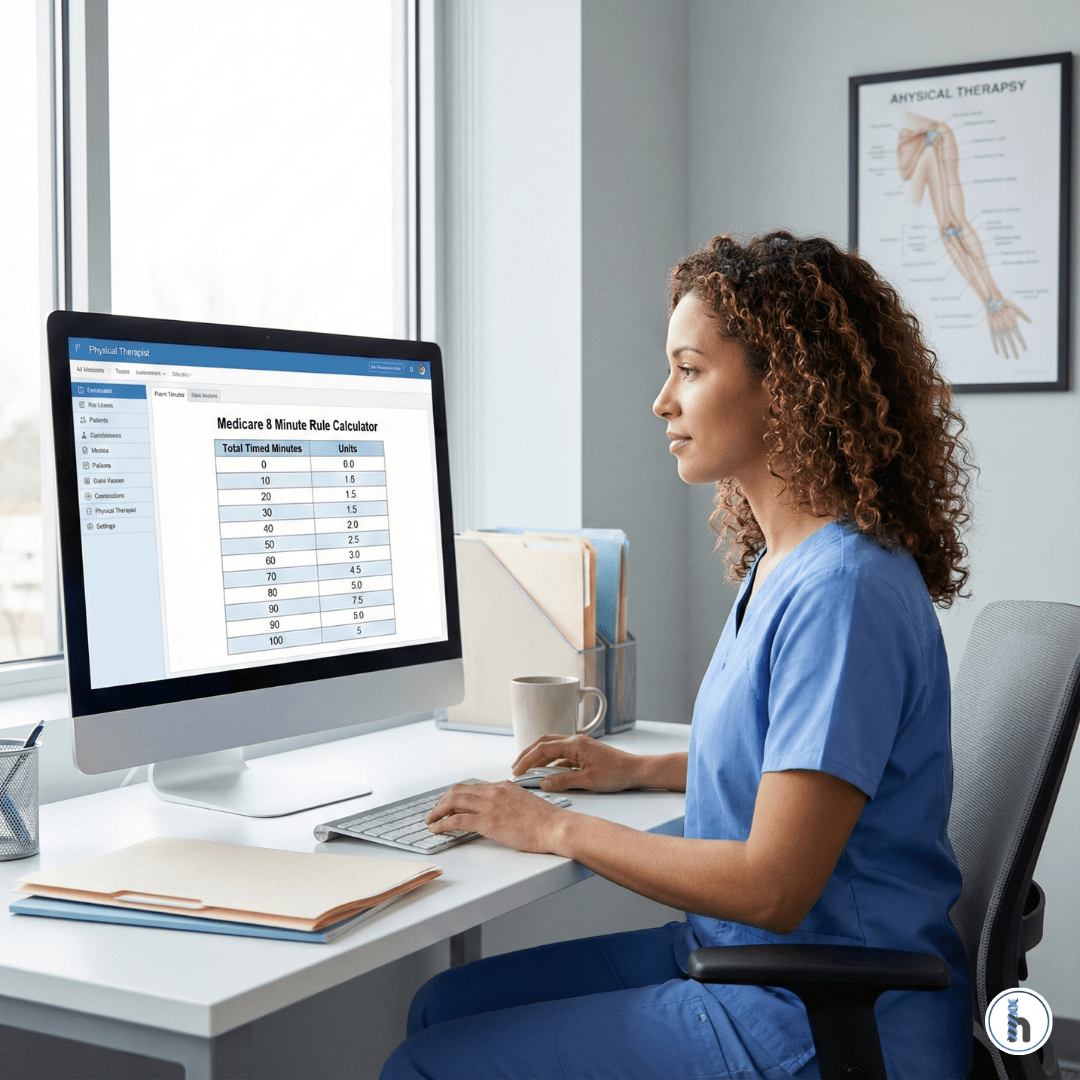
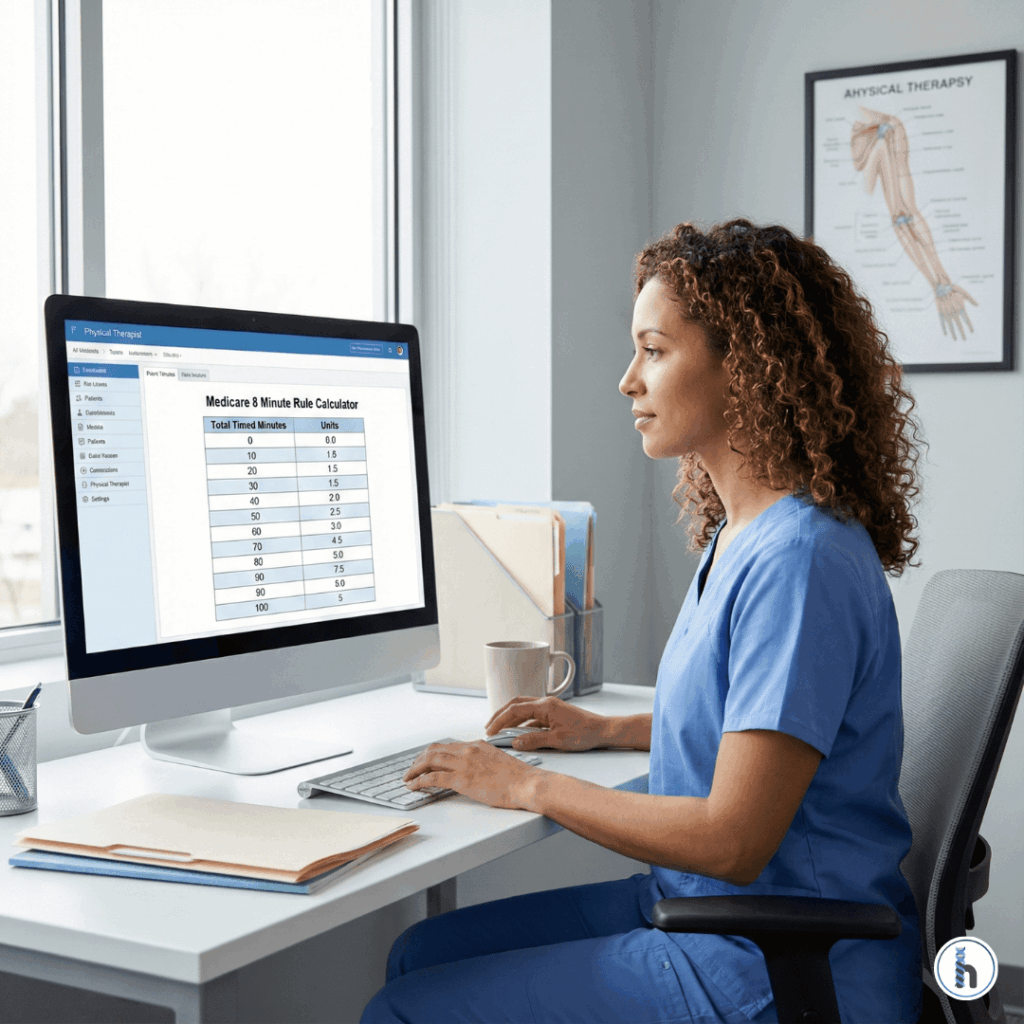
Instead of digging through old charts, HelloNote provides:
Progress percentages
Stagnant-goal indicators
Visual charts for parents and payers
Alerts for reassessment deadlines
Therapists gain confidence because their data is instantly available.
4. Integrated Billing + Compliance Support
HelloNote connects billing and care planning:
Document medical necessity using built-in prompts
Produce audit-ready notes instantly
Maintain compliance across funding sources
This is where care plan software helps protect revenue and reduce denials.
5. Better Patient & Family Engagement
Care plans influence more than treatment they guide communication. HelloNote makes this easy:
Share updated goals
Attach home programs
Provide secure updates
Coordinate with teachers and case managers
When families understand the “why,” adherence improves and so do outcomes.
Real-World Example: Care Plan Software in Action
An SLP working on expressive language can:
Select goals from templates
Track trials live
View automatic progress bars
Generate complete reports with one click
That is efficient care plan software at work faster, clearer, and clinically stronger.
The Business Impact for PT, OT, and SLP Clinics
HelloNote’s care plan features help owners and administrators achieve:
25–40% less documentation time
Lower denial rates
Higher therapist retention
Better team collaboration
Cleaner audit trails
Better care plans → Better outcomes → Better business.
Making the Switch to HelloNote
If your EMR hides your care plan or forces double documentation, upgrading to care plan software that actually supports your workflow is the next step.
HelloNote offers:
Customized onboarding
Discipline-specific templates
Smooth data migration
Workflow training for all team members
Final Thoughts
Care plans shouldn’t get buried they should guide every treatment decision. HelloNote keeps care plans visible, measurable, and integrated into your daily workflow.
Ready to see these features in action?
Schedule a HelloNote Demo Today.
FAQs About Care Plan Software
Care plan software helps therapists create, monitor, and document individualized plans of care while integrating goals into their daily workflow.
It eliminates double documentation, keeps goals visible during note writing, and updates progress in real time.
Yes. Integrated medical-necessity prompts and goal-to-CPT mapping help ensure cleaner, defensible notes.
Yes. HelloNote includes built-in care planning, goal tracking, progress visualization, and billing alignment.
PTs, OTs, SLPs, pediatric therapists, mobile clinicians, and multi-location practices all benefit from streamlined care planning.