Most Commonly Used Modifiers for PT, OT and SLP Services
This article provides a detailed overview of commonly used modifiers in physical, occupational, and speech therapy billing. It explores essential modifiers such as the 59, GP/GO/GN, KX, and GA, with a focus on their application in Medicare and commercial insurance claims. Understand how these modifiers affect reimbursement and ensure accurate billing. Additionally, it discusses how EMR software like HelloNote can simplify billing processes and support proper documentation for compliance.

We have officially arrived into 2021…woohoo, we made it! While a new year may have arrived, some things in the therapy world continue to remain the same. Most, if not all, therapists, whether physical, occupational, or even speech, have entered this career path to improve patients’ lives and make a difference in the lives of those around them. However, it becomes increasingly difficult to continue improving patients’ lives, if you are not billing insurance correctly, resulting in decreased reimbursement and overall profit.
In our last blog post, we discussed the 8-minute billing rule for Medicare, and this time we are going to touch on therapy modifiers for physical, occupational and speech therapy services. What exactly is a modifier? I am glad you asked. A modifier is a code which is added to your billing and provides additional information to the insurance company when diagnosis and procedure codes are not enough for reimbursement. There are two different categories of therapy billing modifiers:
- Therapy modifiers– two-digit codes applied to CPT codes and are typically included when billing both Medicare and commercial insurances
- Level II HCPCS (Healthcare Common Procedure Coding System) Modifiers– two letter codes which are included when billing Medicare, Medicaid and only some commercial plans (such as United Healthcare)
Let’s start by discussing CPT modifiers as there is really only one commonly used modifier for therapy services, which is the 59 modifier. This modifier is used to differentiate between two common or similar services that were provided during the same session. When using the 59 modifier, you are indicating to the insurance company that each service was medically necessary and performed independently of the other. One typical example of when to use this modifier is if you bill for manual therapy (97140) and therapeutic activities (97530), in the same session. As long as you performed each service during separate 15-minute increments, then you would add the 59 modifier on CPT code- 97530 to ensure you receive reimbursement for both codes.
As for level II HCPCS
modifiers, there are three frequently used modifiers, especially for
specific insurances, such as Medicare/Medicaid and more recently, United
Healthcare. Let’s take an individual look at each modifier:
Reference chart below (some common CPT codes if 59 Modifier is allowed. For a full list, please go to National Correct Coding Initiative (NCCI) or consult the official CMS guidelines.
If column 2 shows “Not allowed”, then the CPT code cannot be billed with the code in column 1. If column 2 shows “Yes”, then the 59 modifier can be used to bypass the code edit: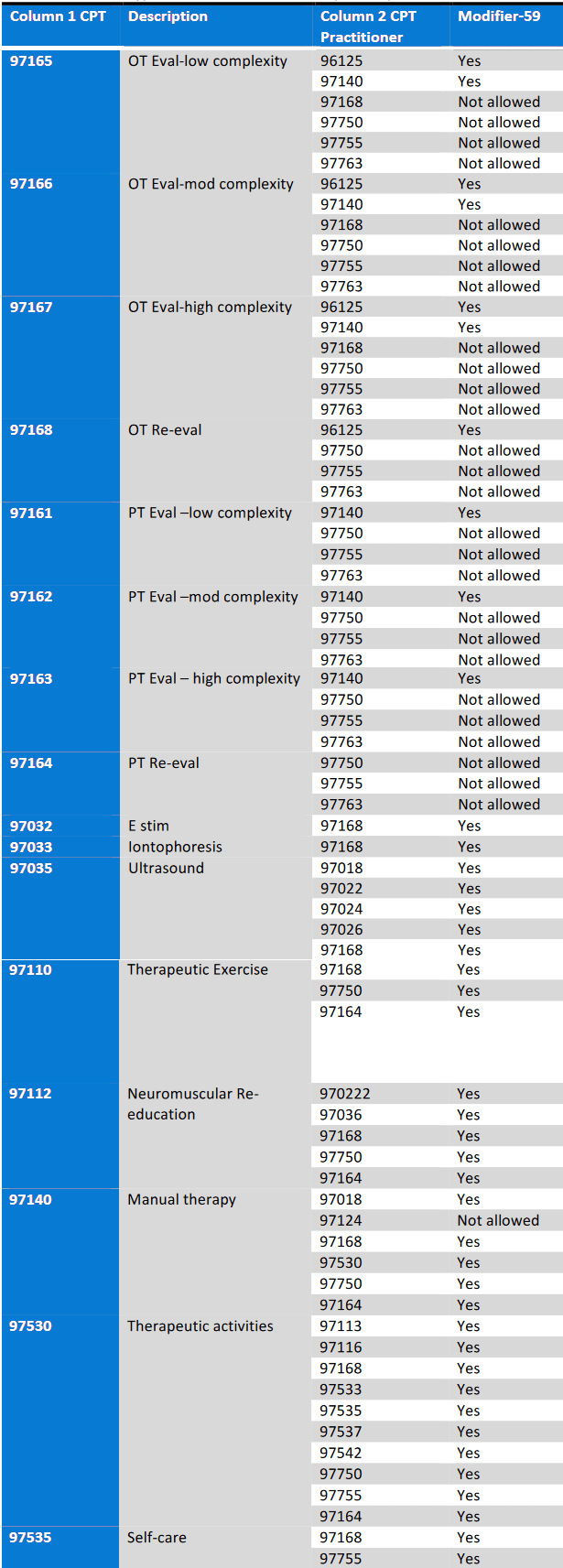
- GP/GO/GN Modifier- This modifier is often used in an interdisciplinary setting where there may be confusion about who provided the services, such as a hospital or outpatient clinic in a physician’s office. When billing for therapy services, be sure to include this modifier so that insurance companies are able to accurately reimburse, based on the type of therapy and in accordance with that member’s group benefits. For physical therapists, use -GP, occupational therapists, use -GO, and speech language pathologists, use -GN.
- KX Modifier- Patients with Medicare insurance have a threshold for therapy services, and once the patient exceeds that threshold, Medicare does not usually reimburse for provided services. In 2021, for PT and SLP services, the combined cap is $2,110 and for OT services, the cap is $2,110. If a patient who is receiving therapy services exceeds this cap, then you would add the KX modifier. Adding this modifier indicates continued treatment is medically necessary and that necessity has been sufficiently justified in your documentation. If using the KX modifier, you do not want to use it before the patient has reached their therapy cap, as that could cause a red flag and lead to a decreased likelihood of approval or reimbursement from Medicare.
- GA Modifier- Last, but not least, is a modifier which is often used once patients have reached a functional plateau, but still wish to receive therapy services. As you know, maintenance therapy is not considered medically necessary so this modifier allows you to bill secondary insurances or bill the patient directly, for non-Medicare covered services. If you end up in a situation where you have to use this modifier, make sure you have communicated with the patient that should they not have any secondary insurance, they will be responsible for paying out-of-pocket for therapy services. By communicating this upfront with your patients, it decreases the likelihood of any confusion or miscommunication.
**One last quick tip, for therapy businesses who have PTAs or OTAs, Medicare now requires that you use an assistant modifier, CQ for PTAs and CO for OTAs, for services performed.
Sometimes insurance is confusing, time consuming or flat out disheartening, but it is important to remember that billing correctly is essential. Modifiers are used to ensure therapists are receiving the appropriate reimbursement from insurance companies so that they can continue to put the patient and their needs first. While modifiers and insurance, in general, can be tricky, consider buying an EMR software that will assist you with your billing, such as HelloNote. As always, remember to support your billing with your documentation, if your notes are not supporting what you are billing insurance for, then you should not be billing for it!

