More Than Muscle Deep: The Science of Massage Therapy and Its Untapped Potential in Rehabilitation and Mental Well Being

Addressing the Whole Patient in Rehabilitation
As physical, occupational, and speech therapists, we’re dedicated to helping patients regain function, mobility, and communication. While we target physical recovery from injuries, surgeries, or health conditions, we often see progress complicated by factors beyond the primary diagnosis. Persistent pain fueled by stress, functional limits increased by anxiety, or recovery stalls linked to mood or sleep issues are common challenges. Recognizing this powerful mind-body connection is vital, suggesting that exploring complementary approaches could significantly enhance our effectiveness.
Understanding the science behind massage therapy in rehabilitation reveals it’s far more than just a tool for relaxation or muscle soreness relief. It possesses a robust scientific foundation demonstrating profound effects on the nervous system and mental state. For rehabilitation professionals and clinic administrators, grasping this science isn’t just academically interesting; it unlocks potential pathways to better patient outcomes, increased engagement, and a more holistic, effective approach to care. This article delves into the mechanisms behind massage therapy and explores its valuable, often underutilized, role in supporting the mental well being of the patients we serve within the rehabilitation context.
The Neurophysiological Symphony: How Massage Influences the Nervous System
The power of skilled touch extends far beyond superficial relaxation. Massage therapy directly influences the autonomic nervous system (ANS), orchestrating a shift away from the sympathetic “fight or flight” state towards the parasympathetic “rest and digest” state. This shift is critical for patients navigating the stresses of recovery and pain. Here’s how:
Stress Hormone Reduction
This is key to understanding how massage reduces cortisol rehabilitation. Research consistently shows that massage therapy decreases levels of cortisol, the body’s primary stress hormone. Chronically elevated cortisol contributes to inflammation, heightened pain perception, muscle tension, impaired tissue healing, and sleep disturbances—all significant barriers in rehabilitation. Lowering cortisol via massage creates a physiological environment more conducive to healing and recovery within the rehabilitation journey.
Boosting “Feel Good” Neurotransmitters
Massage stimulates the release of serotonin and dopamine. Serotonin plays a vital role in mood regulation, anxiety reduction, and promoting feelings of calm. Dopamine is associated with pleasure, motivation, and reward. Increased levels can improve a patient’s mood, outlook, and motivation to participate actively in their therapy program.
Endorphin Release
Massage encourages the production of endorphins, the body’s natural opioids. These neurochemicals act as potent analgesics (pain relievers) and mood elevators, contributing to both physical comfort and emotional uplift.
Vagal Nerve Stimulation
Techniques involving moderate pressure, common in many massage styles, have been shown to increase vagal tone. The vagus nerve is a major component of the parasympathetic nervous system. Enhanced vagal activity promotes relaxation, slows heart rate, reduces inflammation, and improves emotional regulation.
Understanding these mechanisms helps us appreciate that massage isn’t just a passive relaxation technique; it’s an active intervention influencing the neurochemical landscape in ways that directly support therapeutic goals, making it a strong consideration for massage therapy in rehabilitation.
Clinical Relevance for Rehabilitation Populations
The benefits of nervous system regulation via massage have direct applications for common challenges faced by patients in PT, OT, and SLP settings:
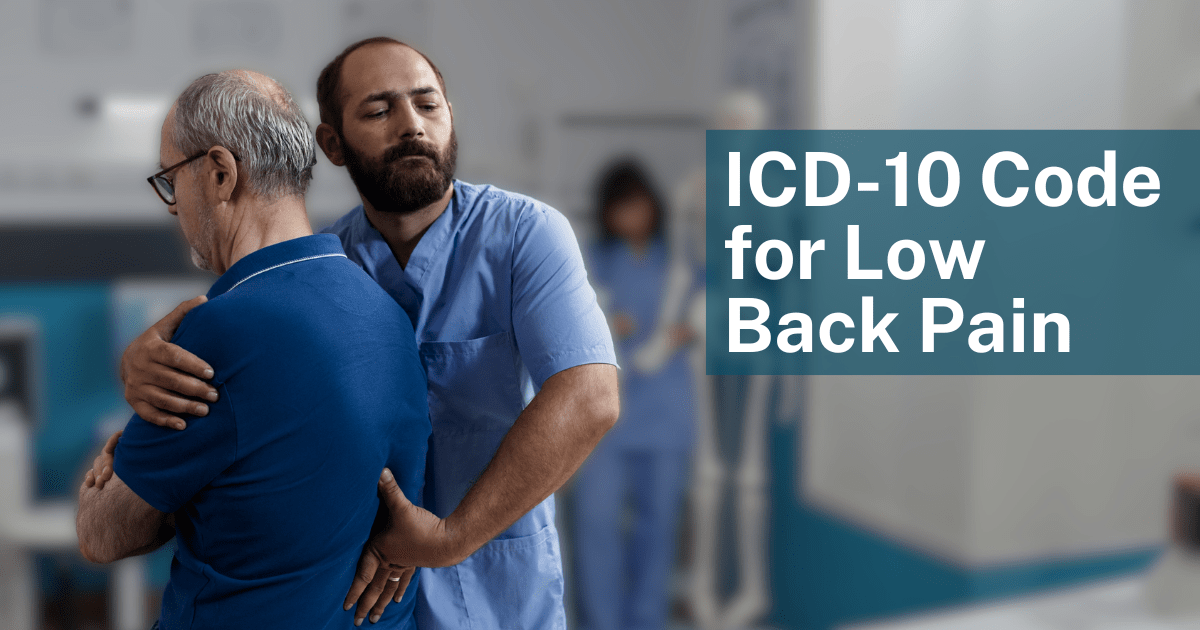
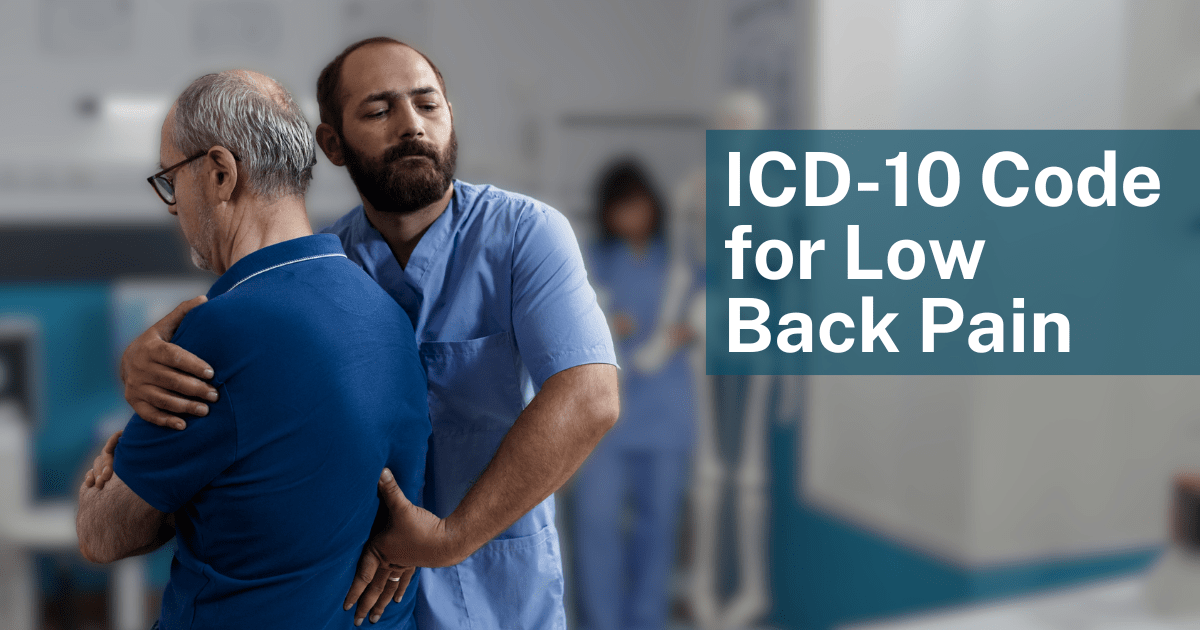
Chronic Pain Management
For patients experiencing conditions like chronic low back pain, fibromyalgia, or arthritis, massage for pain management rehab can be particularly beneficial:
-
-
Massage can help downregulate the nervous system, addressing central sensitization.
-
It aids in reducing persistent muscle guarding and tension.
-
It can decrease the perception of pain.
-
It potentially improves tolerance for therapeutic exercise. Effective massage for pain management rehab requires skilled application tailored to the patient’s condition.
-
Post-Surgical Recovery
Beyond standard PT/OT scar tissue and swelling management:
-
-
Massage can alleviate surgery-related anxiety and stress.
-
It may improve sleep quality, which is crucial for healing.
-
It helps address compensatory muscle tension developed before or after surgery.
-
Neurological Rehabilitation
For patients recovering from stroke, TBI, or managing conditions like MS or Parkinson’s:
-
-
Appropriate massage techniques can help modulate muscle tone and reduce spasticity.
-
It can assist in reducing associated anxiety.
-
It may improve sensory feedback and body awareness.
-
It can enhance body image and acceptance. Considering massage therapy in rehabilitation for neurological conditions requires specific training and precautions.
-
Stress Related Musculoskeletal Complaints
Many patients present with conditions exacerbated by stress, such as tension headaches, temporomandibular joint (TMJ) dysfunction, or postural strain. Massage can directly address the involved musculature while simultaneously mitigating the underlying stress contributing to the symptoms.
Mental Health Comorbidities
Anxiety and depression frequently accompany physical impairments. While massage is not a standalone treatment for these conditions, it can be a powerful adjunct, improving mood, reducing somatic symptoms of anxiety, and enhancing receptiveness to both rehabilitation and mental health interventions.
The Therapeutic Value of Intentional Touch
In a healthcare system often characterized by brief interactions and technological interventions, the simple power of human touch can be profoundly therapeutic. Skilled, intentional touch provided during massage therapy offers:
Proprioceptive Input and Body Awareness
Massage provides rich sensory information, helping patients reconnect with their bodies, improve proprioception (sense of body position), and enhance interoception (sense of internal state), which can be particularly valuable after injury or neurological events.
Non Verbal Communication of Safety
For patients feeling vulnerable, in pain, or anxious, therapeutic touch within a safe, professional context can communicate care, empathy, and safety, helping to calm the nervous system at a fundamental level.
Trauma Informed Potential
Recognizing that many patients may have histories of trauma (medical or otherwise), trauma informed massage approaches prioritize patient control, communication, and nervous system regulation, offering a gentle way to re establish a sense of safety within one’s own body.
Considering Different Massage Modalities
While various techniques exist, some are particularly relevant when considering mental well being and massage therapy in rehabilitation:
-
-
Swedish Massage: Often the foundation, utilizing long, flowing strokes, kneading, and gentle tapping to promote general relaxation, improve circulation, reduce muscle tension, and lower stress levels. Excellent for overall nervous system calming.
-
Myofascial Release (MFR): Focuses on releasing restrictions within the connective tissue (fascia). While often used by PTs/OTs for specific physical limitations, LMTs trained in MFR can address widespread fascial tension that contributes to pain, postural strain, and feelings of physical restriction linked to stress.
-
Craniosacral Therapy (CST): A very gentle technique focused on subtle manipulations of the skull, spine, and pelvis to influence the craniosacral system and promote deep relaxation and nervous system balance. Often sought for stress, headaches, and trauma related issues.
-
Lymphatic Drainage: A gentle technique to support the lymphatic system, relevant post surgery or injury to reduce swelling, but also has calming effects on the nervous system.
-
Neuromuscular Therapy (NMT) / Trigger Point Therapy: Focuses on releasing specific points of muscle hypersensitivity (trigger points) that can refer pain and contribute to chronic tension patterns often exacerbated by stress.
-
The choice of modality often depends on the patient’s specific needs, preferences, and the therapist’s training.
Integrating Massage into the Rehabilitation Ecosystem
How can rehabilitation clinics effectively leverage the benefits of massage therapy?
Develop Referral Networks
Build relationships with qualified, licensed massage therapists (LMTs) in your community who understand rehabilitation principles and ideally have experience with relevant patient populations (e.g., oncology massage, neuro massage, orthopedic massage). Clear communication about patient goals is key.
Consider In House Services
Some larger clinics or wellness centers may employ LMTs directly. This allows for closer collaboration and seamless integration into patient care plans, but requires careful consideration of space, scheduling, and management. This model optimizes the use of massage therapy in rehabilitation settings.
Patient Education
Inform patients about the potential benefits of massage as a complement to their primary rehabilitation therapy, particularly for managing stress, pain (where massage for pain management rehab is relevant), and improving overall well being related to their recovery.
Scope Awareness
Clearly differentiate between the manual therapy techniques performed by PTs/OTs within their scope (often focused on specific joint/tissue mobilization for functional goals) and the broader relaxation, stress reduction, and systemic effects often targeted by LMTs.
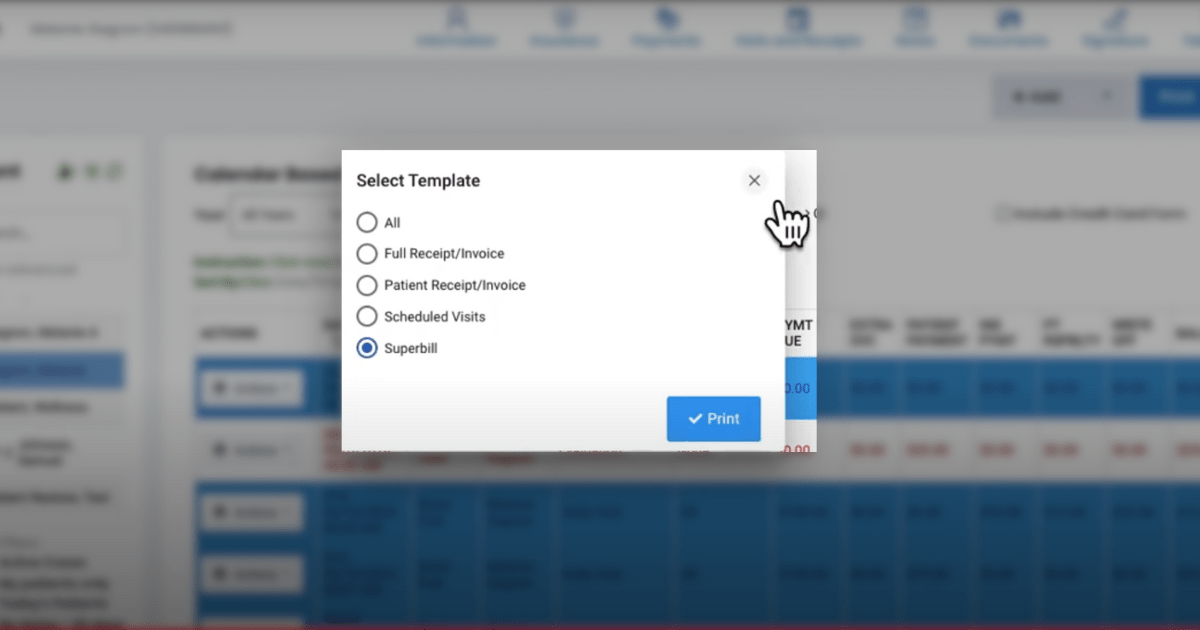
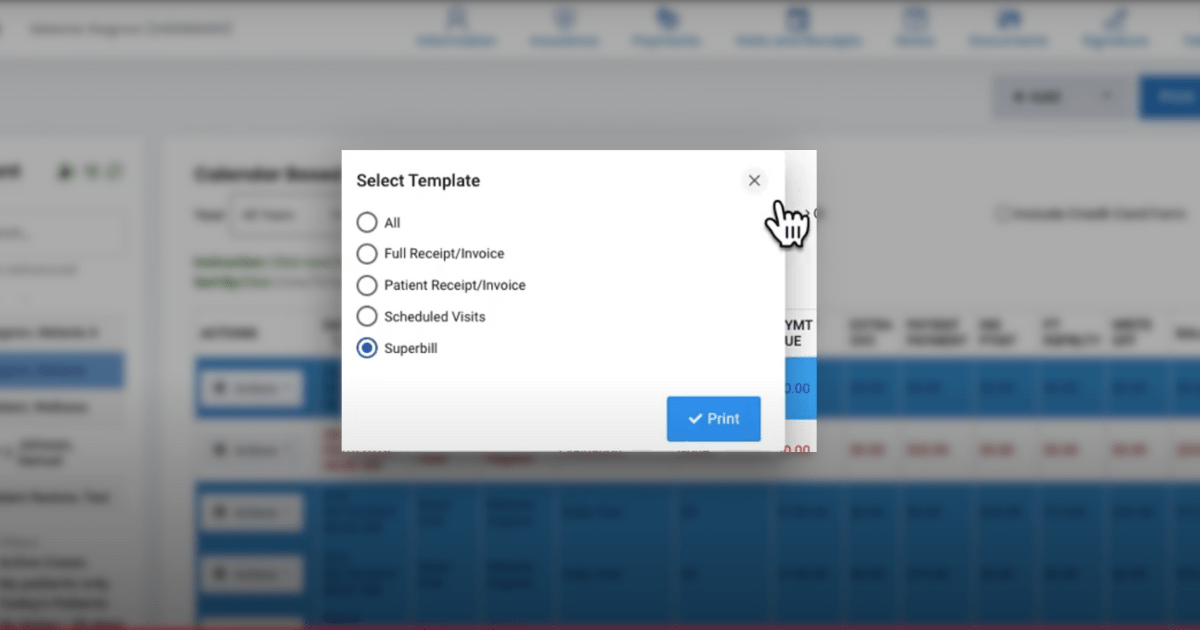
Efficient Documentation and Coordination: The HelloNote Advantage
Whether referring out or employing LMTs, managing information and coordinating care efficiently is crucial. This is where a versatile Electronic Medical Record (EMR) system like HelloNote becomes invaluable:
-
-
Tracking Referrals: Easily document referrals made to LMTs, including the reason for referral and communication sent, maintaining a comprehensive patient record.
-
Integrated Documentation (for In House LMTs): If employing LMTs, HelloNote can provide customizable templates (e.g., SOAP notes tailored for massage) allowing them to document sessions within the same patient chart, facilitating easy review by the primary rehab therapist.
-
Monitoring Patient Response: Rehab therapists can use HelloNote to document patient reported feedback on massage interventions and objectively track changes in pain levels, range of motion, functional scores, or goal achievement that may correlate with the addition of massage therapy.
-
Secure Inter provider Communication: Utilize secure messaging features within HelloNote to communicate (with patient consent) relevant information or progress updates between the rehab therapist and the LMT, ensuring continuity of care.
-
Goal Alignment: Document how adjunctive massage therapy supports specific rehabilitation goals (e.g., “Patient receiving weekly massage to manage stress and muscle tension, supporting improved participation in therapeutic exercise program”).
-
HelloNote helps streamline these processes, ensuring that integrating massage therapy enhances, rather than complicates, clinical workflow and supports quality patient care.
Discover how HelloNote’s features support integrated care models in your clinic.