Superbill for Therapy: A Complete Guide for Cash-Based Practices
Learn how a superbill for therapy can help cash-based practices provide patients with out-of-network reimbursement options while maintaining financial independence. Discover best practices for superbill documentation, reimbursement strategies, and how EMR systems streamline the process.
Understanding the Role of Superbills in Therapy Practices
In a cash-based therapy practice, managing financial transactions efficiently is crucial for both providers and patients. One essential document that facilitates this process is the superbill. While many therapy practices operate outside traditional insurance networks, a superbill serves as a bridge, allowing patients to seek reimbursement from their insurance providers while enabling therapists to maintain an independent practice model.
A superbill is a detailed receipt that a therapist provides to a patient after a session. Unlike a standard invoice, it includes critical information necessary for insurance claims, such as procedure codes, diagnosis codes, provider details, and the total amount charged. Patients submit this document to their insurance companies to request partial or full reimbursement for out-of-network services.
Key Components of a Superbill
A properly structured superbill contains the following essential elements:
-
- Provider Information: The therapist’s name, practice name, address, National Provider Identifier (NPI), and tax ID.
-
- Patient Information: The full name and date of birth of the patient receiving the service.
-
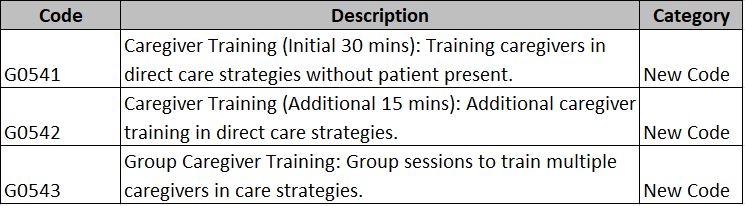
- Service Details: The date of service, description of the therapy provided, and corresponding Current Procedural Terminology (CPT) codes.
-
- Diagnosis Code: The International Classification of Diseases (ICD) code that justifies the treatment.
-
- Billing Amount: The total charge for the service.
-
- Payment Details: The amount paid by the patient, confirming that they have covered the cost upfront.
- Provider Signature: A signature from the therapist validating the document.
Why Cash-Based Therapy Practices Use Superbills
Therapists who operate outside insurance networks often use superbills to help patients access reimbursement while maintaining financial autonomy. Here’s why superbills are an integral part of cash-based therapy practices:
-
- Enables Patients to Use Insurance Benefits
Many patients prefer out-of-network therapy providers but still want to use their insurance benefits. By submitting a superbill, they can seek reimbursement for a portion of their therapy expenses, reducing their out-of-pocket costs.
-
- Allows Therapists to Avoid Insurance Hassles
Therapists who opt for a cash-based model can avoid the administrative burden and payment delays associated with insurance billing. Instead of dealing with complex claims and insurance denials, they can focus on providing quality care while still supporting patients in leveraging their benefits.
-
- Encourages Financial Transparency
A superbill provides a clear breakdown of charges, ensuring that patients understand the cost of their therapy sessions. This transparency fosters trust between the therapist and the client.
-
- Expands Access to Therapy
Since some insurance plans partially reimburse for out-of-network services, superbills make therapy more financially feasible for patients who might not otherwise afford it.
How to Create a Professional and Compliant Superbill
For a superbill to be valid and accepted by insurance providers, it must be structured correctly. Here are some best practices for generating a high-quality superbill:
-
- Ensure Accuracy: Double-check all details, especially CPT codes and diagnosis codes, to prevent claim denials.
-
- Maintain HIPAA Compliance: Protect patient data and ensure that the superbill complies with privacy regulations.
-
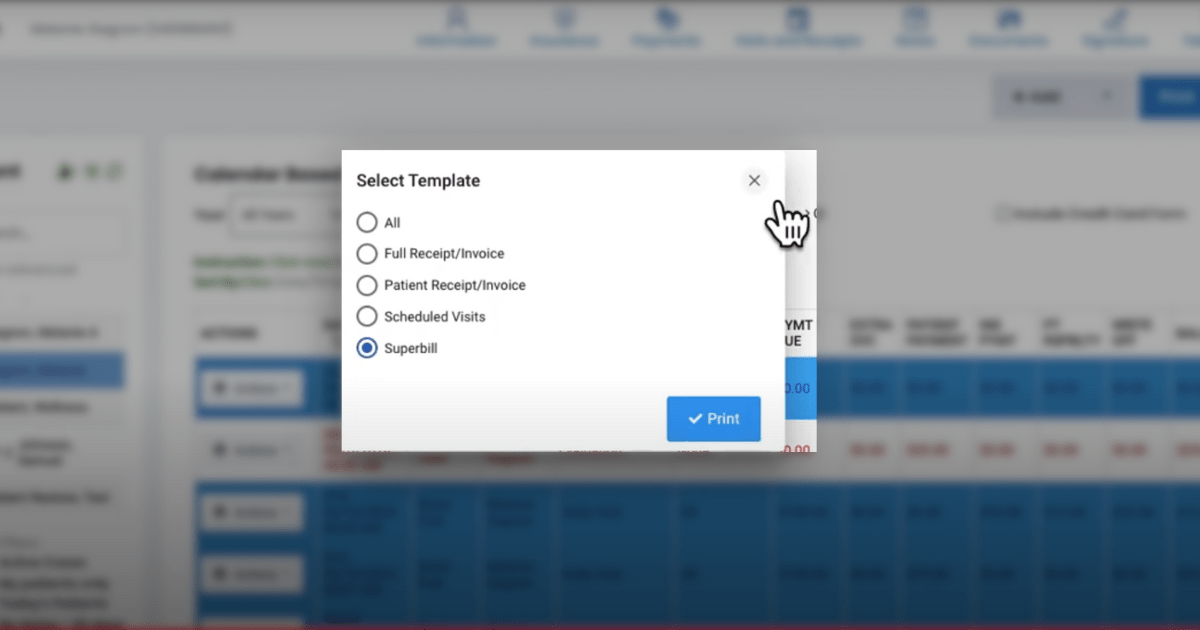
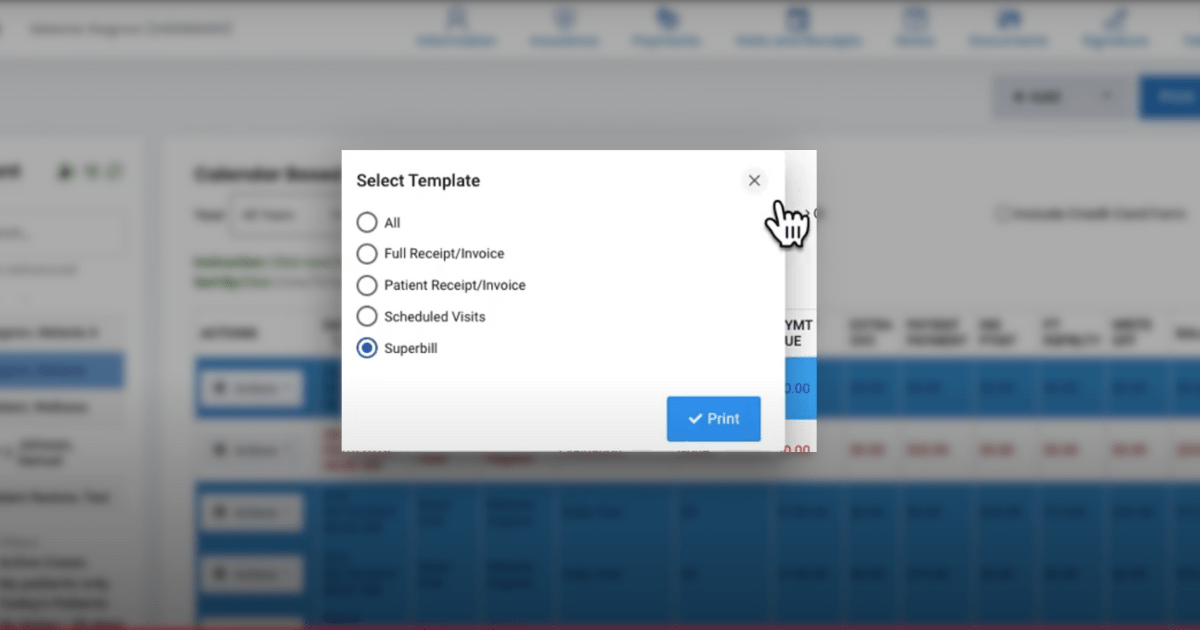
- Use a Digital System: Many therapy practices use Electronic Medical Records (EMR) or practice management software to generate superbills quickly and accurately.
-
- Educate Patients: Provide a simple guide on how they can submit the superbill to their insurance company, along with any necessary supporting documents.
Common Challenges and Solutions When Using Superbills
Challenge 1: Patients May Struggle with Insurance Claims
Some patients may be unfamiliar with the process of submitting a superbill to their insurance provider, leading to confusion and delays.
Solution: Offer a clear, step-by-step guide explaining how they can file a claim and what to expect during the reimbursement process.
Challenge 2: Insurance Denials
Not all insurance plans reimburse out-of-network services, and some may reject claims due to missing information or incorrect codes.
Solution: Encourage patients to check with their insurance provider before starting therapy. Additionally, provide accurate and complete information on the superbill.
Challenge 3: Managing Superbills Efficiently
For therapists handling multiple patients, manually generating superbills can be time-consuming.
Solution: Use EMR software or billing platforms that automate the superbill creation process, reducing administrative workload.
The Future of Superbills in Therapy Practices
As more therapists transition to cash-based models, the demand for streamlined superbill processing continues to grow. Emerging digital solutions, such as integrated billing software, are making it easier for both therapists and patients to handle superbills effectively. Moreover, increasing awareness about out-of-network reimbursement options is empowering patients to seek therapy from providers who best meet their needs.
Conclusion
A superbill is an essential tool for cash-based therapy practices, allowing therapists to offer services without direct insurance involvement while enabling patients to seek reimbursement. By understanding how to create and manage superbills effectively, therapy providers can enhance their practice operations, improve patient satisfaction, and maintain financial stability.
If you’re a therapist running a cash-based practice, implementing a well-structured superbill system can simplify billing, support your clients, and ultimately contribute to the success of your business.