KX Modifier 2025 Explained: Optimize Therapy Billing and Compliance
Simplify therapy billing with this comprehensive guide to the KX Modifier. Learn how it ensures compliance, supports medical necessity, and streamlines reimbursements.

January marks the beginning of a new year and a fresh opportunity to optimize your therapy practice’s billing and compliance processes. Therapy modifiers, including Medicare’s KX modifier and state-imposed limits, are essential tools for ensuring accurate billing and securing reimbursement. While some modifiers, like the KX modifier, may not be immediately relevant at the start of the year, preparing for their eventual use can help avoid disruptions and ensure a smooth workflow as the year progresses.
This article explores why therapy modifiers matter, the challenges they present, and how you can set your practice up for success in 2025.
Why Modifiers Matter in Therapy Billing
Modifiers provide additional context for therapy billing, helping payers understand the specifics of the services being provided. Proper use of these codes ensures accurate claim processing, minimizes the risk of denials, and keeps your practice compliant.
Common Therapy Modifiers
- KX Modifier: Indicates therapy services exceeding Medicare’s annual threshold are medically necessary.
- GA Modifier: Signifies that an Advance Beneficiary Notice (ABN) was issued to notify the patient of potential non-coverage.
- 59 Modifier: Prevents claim bundling by identifying distinct services provided on the same day.
- CQ Modifier: Identifies physical therapy services delivered by a physical therapist assistant (PTA).
- GP Modifier: Specifies services delivered under a physical therapy plan of care.
- CO Modifier: Applies to occupational therapy services provided by an occupational therapy assistant (OTA).
- GN Modifier: Reflects speech-language pathology services under a therapy plan of care.
Accurate application of these modifiers is critical for compliance and securing timely reimbursement.
State-Imposed Therapy Limits: Staying Ahead
State-imposed limits on therapy services add another layer of complexity for providers. These restrictions, such as session limits or coverage criteria, vary widely and require close monitoring to avoid issues.
Common Challenges with State-Imposed Limits
- Variable Rules: Different states and payers have varying therapy limits, making it challenging to stay updated.
- Patient Disruptions: Exceeding limits can lead to denied claims, forcing patients to pay out-of-pocket or delay care.
- Administrative Burden: Tracking usage against limits while managing a busy caseload adds complexity.
How to Stay Ahead
- Verify Benefits Early: At the start of the year, confirm patient benefits and therapy limits to plan treatment effectively.
- Monitor Usage: Use EMR tools to track therapy sessions and ensure they remain within allowable limits.
- Proactive Communication: Keep patients informed about their coverage and discuss alternative options if their benefits may run out.
The KX Modifier: Preparing for Its Use Later in the Year
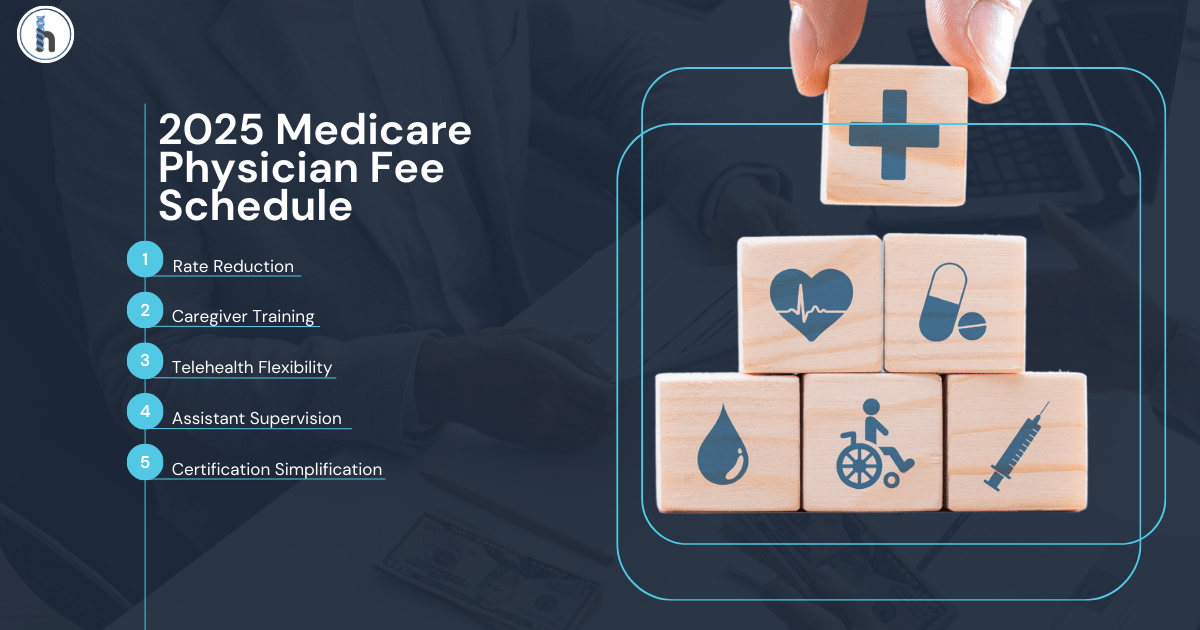
The KX modifier is a crucial tool for Medicare billing, allowing services to continue beyond Medicare’s annual therapy thresholds. However, it’s typically applied later in the year when patients begin to exceed these thresholds. For 2025, the Medicare therapy thresholds are:
- $2,230 for combined physical therapy and speech-language pathology services.
- $2,230 for occupational therapy services.
Why the KX Modifier Isn’t Relevant in January
At the beginning of the year, therapy services rarely exceed the annual thresholds, so the KX modifier is not immediately required. Instead, January is an ideal time to focus on:
- Understanding Thresholds: Familiarize yourself with Medicare’s limits and ensure your documentation supports claims that may require the KX modifier later in the year.
- Setting Up Tracking Systems: Establish systems to monitor cumulative therapy costs and identify when patients are approaching their thresholds.
Using the KX Modifier Effectively
When thresholds are reached later in the year:
Document Thoroughly: Justify the medical necessity of continued therapy with clear and comprehensive notes.
Monitor Progress: Ensure that ongoing therapy aligns with patient goals and Medicare’s guidelines for medical necessity.
Automate Compliance: Use an EMR system to apply the KX modifier accurately and eliminate manual tracking.
A Time for Preparation and Process Optimization
Now is the time to prepare for its eventual use and ensure your practice is ready for the year ahead.
Steps to Take in January
Review 2024 Trends: Analyze last year’s claim denials and modifier-related issues to identify areas for improvement.
Train Your Team: Ensure that everyone on your staff understands how and when to use modifiers, including the KX modifier.
Implement Monitoring Tools: Use tools like HelloNote EMR to track therapy thresholds and modifier usage seamlessly.
How HelloNote EMR Simplifies Modifier Management
Navigating therapy modifiers like the KX modifier can feel overwhelming, but HelloNote EMR makes the process manageable and efficient.
Key Features of HelloNote EMR
Automatic Alerts: Receive notifications when patients approach Medicare thresholds, allowing you to prepare for KX modifier application.
Integrated Modifier Tools: Apply modifiers like KX, GA, and 59 with ease using guided prompts that reduce errors.
Comprehensive Reporting: Track therapy sessions, modifier usage, and compliance, making audits and appeals straightforward.
Team Collaboration: Share updates with your team to ensure everyone is aligned on patient progress and compliance requirements.
With HelloNote, you can eliminate unnecessary steps and focus on what matters most: providing exceptional care to your patients.
Set the Tone for Success in 2025
While the KX modifier won’t be needed early in the year, understanding its purpose and preparing your processes will save you time and stress as thresholds are reached later on. By leveraging tools like HelloNote EMR, you can streamline billing, maintain compliance, and focus on delivering quality care.
Ready to simplify modifier management and improve your practice’s efficiency?
Schedule a demo with HelloNote today to learn how our platform can help you stay ahead of billing challenges and achieve your goals in 2025. Let’s make this your best year yet!