Therapeutic Exercises CPT Code 97110: A Complete Guide to Billing, Documentation, and Reimbursement
Learn everything about CPT Code 97110, the essential billing code for therapeutic exercise in physical, occupational, and speech therapy. Discover its correct usage, documentation requirements, Medicare compliance, and best practices to maximize reimbursement while avoiding claim denials.
Introduction
CPT Code 97110 is one of the most used billing codes in physical therapy, occupational therapy, and speech-language pathology for therapeutic exercises aimed at improving patient function. This code plays a critical role in rehabilitation by addressing strength, endurance, range of motion, and flexibility.
Understanding when and how to use CPT Code 97110 ensures accurate billing, Medicare compliance, and maximum reimbursement. This guide covers when to use CPT 97110, documentation requirements, key differences from other therapy codes, billing rates, a comparison with similar codes, and billing best practices to avoid claim denials.
What Is CPT Code 97110?
Definition
CPT Code 97110 is defined as:
This code is used for individualized, structured exercises that improve a patient’s physical abilities. The exercises must be designed to address specific impairments and contribute to the patient’s functional goals.
Key Features of CPT 97110:
-
- Hands-on, one-on-one therapy
-
- Focus on improving movement, strength, and function
-
- Billed in 15-minute increments
-
- Requires measurable improvement and patient participation
Billing Rates for CPT 97110
Billing rates for CPT 97110 vary depending on location, payer, and provider contracts. On average, Medicare reimburses approximately $30 to $40 per 15-minute unit, while private insurers may reimburse between $35 to $50 per unit. It’s essential for therapy practices to verify reimbursement rates with specific payers and ensure accurate coding to maximize revenue.
When to Use CPT Code 97110?
Common Conditions Treated
Therapists may use 97110 for a wide range of diagnoses, including:
-
- Orthopedic injuries (fractures, post-surgical rehabilitation, joint replacements)
-
- Neurological conditions (stroke, spinal cord injury, Parkinson’s disease)
-
- Chronic pain syndromes (fibromyalgia, arthritis)
-
- Pediatric therapy (developmental delays, motor coordination deficits)
Examples of Therapeutic Exercises Under 97110
CPT Code 97110 applies when specific, structured exercises are prescribed for a functional goal. Examples include:
-
- Leg press exercises to strengthen lower limbs post-knee replacement
-
- Shoulder range-of-motion drills after rotator cuff surgery
-
- Grip-strength exercises for post-stroke rehabilitation
-
- Core stabilization exercises for chronic low back pain
-
- Flexibility training to improve joint mobility after immobilization
Comparison of CPT 97110 vs. Other Therapy Codes
Therapists must differentiate between CPT 97110 (therapeutic exercises) and other similar therapy codes to ensure proper billing.
|
CPT Code |
Description |
Example Use Case |
|
97110 |
Therapeutic exercises for strength, endurance, and flexibility |
Leg press after knee replacement |
|
97112 |
Neuromuscular re-education for balance, coordination, and proprioception |
Balance training for stroke recovery |
|
Therapeutic activities that simulate functional tasks |
Sit-to-stand training for daily mobility |
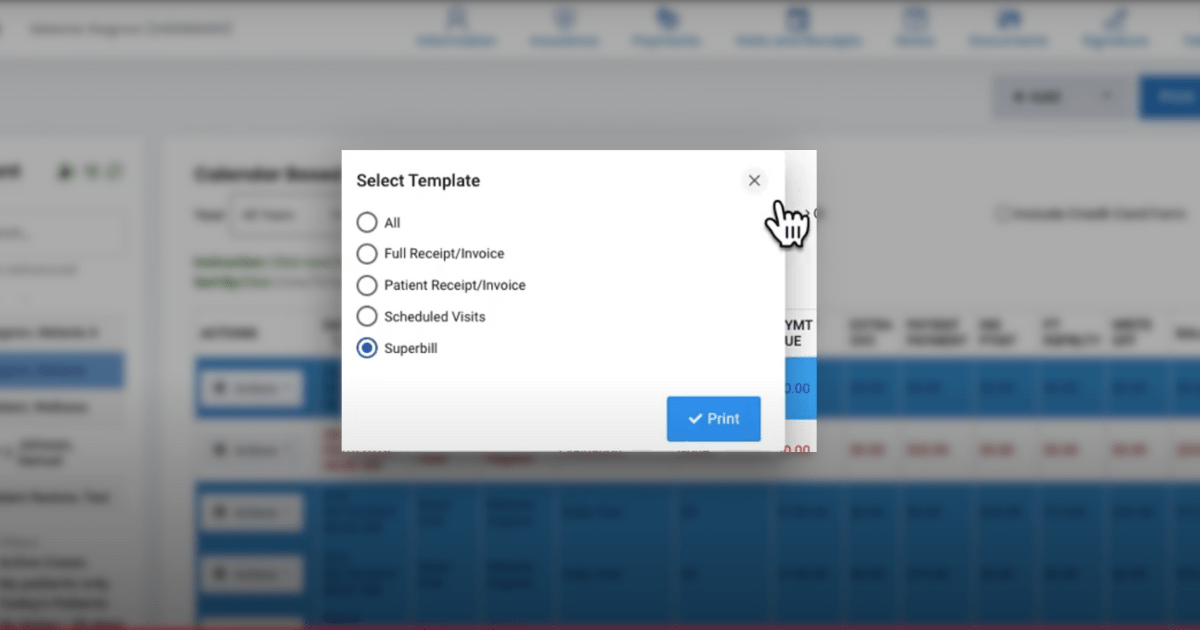
Billing and Documentation for CPT 97110
Billing Guidelines
-
- Billed in 15-minute increments (minimum 8 minutes per unit)
-
- Requires direct one-on-one interaction with the therapist
-
- Cannot be billed on the same day as 97530 unless separate goals/body parts are addressed
-
- Must document medical necessity and progress toward goals
Medicare and Insurance Compliance
Medicare and private insurers require thorough documentation to justify reimbursement for 97110. Therapists should include:
-
- The specific exercises performed
-
- The functional goal of the exercise
-
- Patient response to treatment and measurable progress
-
- Adaptive equipment used (e.g., resistance bands, dumbbells)
Example documentation entry:
“Patient performed resisted shoulder flexion exercises using a 2 lb weight to increase strength for independent dressing. Required minimal assistance. Goal: Improve ability to lift arms overhead for self-care tasks within 4 weeks.”
Avoiding Common Denials for CPT Code 97110
- Insufficient Documentation
Many claim denials occur due to lack of clear documentation. Avoid vague entries like: “Patient performed strength exercises.” Instead, specify: “Patient completed 3 sets of 10 repetitions of quadriceps exercises using a resistance band to improve knee stability for walking.”
- Billing 97110 and 97530 Together Without Justification
If billing 97110 (therapeutic exercises) and 97530 (therapeutic activities) on the same day, documentation must differentiate them: 97110 is for specific muscle training (e.g., resistance training for knee strength) 97530 is for functional training (e.g., car transfer simulation)
- Using Modifier 59 for 97110 and 97530 on the Same Day
When billing 97110 and 97530 together, Modifier 59 must be used to indicate that these services were distinct and separately identifiable. Modifier 59 tells payers that the two codes were used for different therapeutic purposes, reducing the risk of claim denials.
Example of Correct Billing with Modifier 59: “Patient completed therapeutic exercises (97110) to strengthen knee extensors for improved gait. Separately, the patient performed functional sit-to-stand training (97530) to improve independence in daily mobility. Modifier 59 applied to distinguish separate goals.”
Avoid Overuse: Modifier 59 should only be applied when documentation clearly supports separate treatment purposes. Improper use may trigger audits or payment rejections.
Case Study: Resolving a Claim Denial for 97110
A physical therapy clinic submitted a claim for 97110 and 97530 on the same day without proper documentation. The claim was denied due to lack of differentiation between the two codes. After reviewing the documentation, the clinic resubmitted the claim with a clear distinction between the therapeutic exercises (97110) and functional training (97530), using Modifier 59 correctly. As a result, the insurance provider approved the claim upon reconsideration.
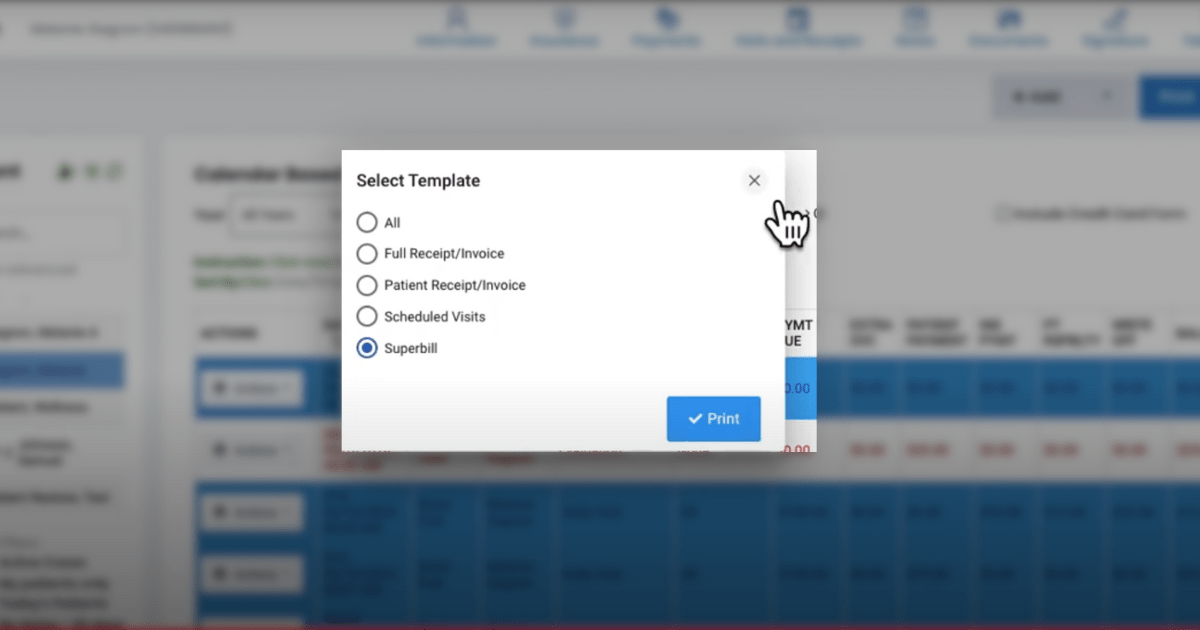
How HelloNote EMR Simplifies CPT 97110 Billing
Accurate billing and documentation can be complex and time-consuming, but HelloNote EMR streamlines the process by: Automating CPT code selection to ensure correct billing for therapeutic exercises Providing built-in compliance alerts to guide therapists on proper use of Modifier 59 when billing 97110 with other therapy codes Tracking patient progress with real-time documentation and reporting tools Reducing administrative burden by integrating scheduling, documentation, and billing in one system
By using HelloNote EMR, therapy practices can improve claim approval rates, prevent denials, and enhance overall practice efficiency.
Final Thoughts
CPT Code 97110 is essential for billing structured therapeutic exercises in physical therapy, occupational therapy, and speech-language pathology. Understanding when and how to use it correctly ensures proper reimbursement, compliance with Medicare and insurance policies, and optimal patient care.
By following best documentation practices, using Modifier 59 when necessary, and leveraging an EMR like HelloNote, therapists can streamline their billing processes, maximize reimbursement, and avoid costly claim denials.