Best EMR Software for Regulatory Compliance: Keeping Healthcare Practices Ahead
Looking for the best EMR software for regulatory compliance? Ensure your practice stays ahead with a system that offers HIPAA-compliant security, automated billing accuracy, seamless interoperability, and real-time updates for evolving healthcare regulations. Learn how the right EMR can help you protect patient data, reduce claim denials, and streamline compliance efforts effortlessly.
The healthcare industry operates in a highly regulated environment, where compliance with evolving laws and standards is not just a recommendation, it’s a necessity. Electronic Medical Record systems play a crucial role in ensuring that healthcare providers meet these regulations, but keeping them updated, secure, and compliant requires continuous monitoring and proactive updates.
From HIPAA privacy laws to Medicare documentation requirements, failing to comply with healthcare regulations can lead to financial penalties, security breaches, and loss of patient trust. In this article, we’ll explore why regulatory compliance in EMRs is essential, discuss the most critical updates providers must monitor, and highlight how healthcare organizations can ensure their EMR systems remain up to date.
Why Regulatory Compliance Matters in EMR Systems
An EMR system is more than just a digital filing cabinet for patient records, it is an essential tool for managing compliance, documentation, and data security. With regulations constantly evolving, healthcare providers must ensure that their EMRs are updated to meet:
-
- Data security requirements – Protecting patient health information (PHI) under HIPAA and other privacy laws.
-
- Billing and coding updates – Aligning with Medicare, Medicaid, and private insurer requirements to avoid claim denials.
-
- Quality reporting standards – Meeting value-based care models such as MIPS (Merit-Based Incentive Payment System).
-
- Interoperability and data-sharing rules – Ensuring seamless exchange of patient records under the 21st Century Cures Act.
Without regular EMR updates, providers risk compliance violations, legal repercussions, and operational inefficiencies that could impact both patient care and financial stability.
Key Regulatory Compliance Areas for EMR Systems
1. HIPAA & Patient Data Security
The Health Insurance Portability and Accountability Act (HIPAA) mandates strict safeguards for electronic patient records, ensuring that EMRs protect sensitive data from breaches, unauthorized access, and cyber threats.
EMRs Must Support:
-
- End-to-end encryption for data transmission and storage.
-
- User access controls to prevent unauthorized data exposure.
-
- Audit logs and security tracking for HIPAA compliance audits.
-
- Automatic backups and disaster recovery to prevent data loss.
Recent Update: The HHS Office for Civil Rights (OCR) has proposed stricter patient access rules, requiring EMRs to facilitate easier sharing of records while maintaining security compliance.
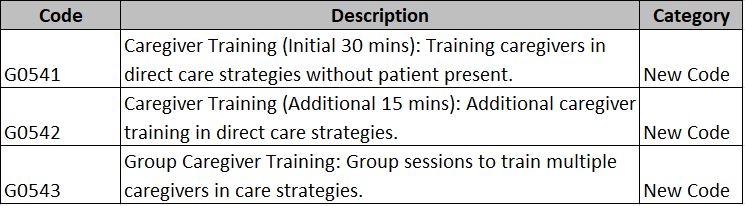
2. Medicare & Medicaid Compliance
EMRs must align with Medicare and Medicaid guidelines to ensure that providers can properly document patient encounters, submit claims accurately, and receive timely reimbursements.
EMRs Must Support:
-
- FHIR (Fast Healthcare Interoperability Resources) APIs for Data-Sharing
A standardized framework enabling real-time exchange of patient data with hospitals, labs, and insurance networks.
Example: A primary care physician refers a patient to a physical therapist. With FHIR-enabled EMRs, the therapist can instantly access the patient’s medical history, test results, and imaging scans.
-
- Patient Access to Records via Secure Portals
Compliance with HIPAA and the Cures Act by providing patients direct access to their health records.
Example: A physical therapy patient recovering from a knee injury can log into their HelloNote patient portal to review rehabilitation exercises, progress notes, and upcoming session details.
-
- Compliance with the Trusted Exchange Framework and Common Agreement (TEFCA)
Ensuring healthcare providers can securely access and share patient records across different facilities.
Example: A patient undergoing chronic pain management sees multiple specialists. A TEFCA-compliant EMR ensures all providers have access to the same updated treatment records.
Recent Update: Medicare’s 2025 reimbursement models emphasize value-based payments, requiring EMRs to track patient outcomes and quality measures rather than just service volume.
3. The 21st Century Cures Act & Interoperability
Interoperability—the ability of different healthcare systems to securely share patient information—is a key regulatory focus. The 21st Century Cures Act mandates that EMRs allow seamless data exchange while preventing information blocking.
EMRs Must Support:
-
- FHIR (Fast Healthcare Interoperability Resources) APIs for Data-Sharing
Enhancing communication between EMRs and healthcare platforms to improve care coordination.
-
- Patient Access to Records via Secure Portals
Allowing patients to view treatment history, schedule appointments, and securely communicate with providers.
-
- Compliance with TEFCA
Standardizing health data exchange to improve efficiency and patient safety.
Recent Update: In 2025, non-compliant EMR vendors will face penalties for restricting data-sharing or limiting patient access to health records.
4. Compliance with Telehealth & Remote Care Regulations
With the rise of telehealth, EMRs must now support secure virtual care features that comply with state and federal laws.
EMRs Must Support:
-
- HIPAA-compliant video conferencing and secure patient messaging.
-
- Telehealth reimbursement tracking for Medicare & private insurers.
-
- Digital consent forms for remote patient interactions.
Recent Update: Medicare’s 2025 Telehealth Expansion will continue allowing remote physical therapy, occupational therapy, and speech-language pathology services, requiring EMRs to have telehealth documentation support.
How Healthcare Organizations Can Ensure EMR Compliance
-
- Choose an EMR with Built-In Compliance Updates
Opt for an EMR that automatically updates for regulatory changes.
Use cloud-based EMRs that don’t require manual software updates or IT maintenance.
-
- Conduct Regular Compliance Audits
Review EMR security settings to ensure HIPAA compliance.
Monitor billing accuracy to prevent claim denials.
Check interoperability capabilities to avoid violations.
-
- Train Staff on New Regulations
Schedule compliance training sessions for staff.
Assign a compliance officer or EMR administrator to oversee regulatory adherence.
-
- Utilize Vendor Support for Compliance Guidance
Work with an EMR vendor that provides regular compliance updates and customer support.
Request training on new regulatory features to ensure proper usage.
How HelloNote Ensures Compliance for Therapy Practices
At HelloNote, we prioritize compliance and regulatory updates so that therapy providers can focus on patient care rather than administrative burdens.
-
- Automatic Updates for Healthcare Regulations – Keeping documentation, billing, and security settings up to date.
-
- HIPAA-Compliant Security Features – Encrypted data storage, role-based user access, and audit tracking.
-
- Integrated Medicare & Insurance Billing Compliance – ICD-10, CPT, and 8-minute rule support to reduce claim denials.
-
- Seamless Interoperability – FHIR API compatibility for secure data-sharing.
-
- Telehealth Documentation Support – Secure video conferencing and telehealth billing tools built for therapy professionals.
Looking for an EMR that keeps you ahead of compliance updates? Book a Free Demo of HelloNote Today!
The Future of EMR Compliance
As healthcare regulations evolve, EMRs must continuously adapt to ensure compliance, security, and efficiency. Providers who invest in compliance-focused EMR systems will be better equipped to reduce legal risks, maximize reimbursements, and improve patient outcomes.